Nerve Block or Gel? Comparing Analgesia Techniques for Enhancing Comfort During Trans-Rectal Ultrasound-Guided Prostate Biopsy
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
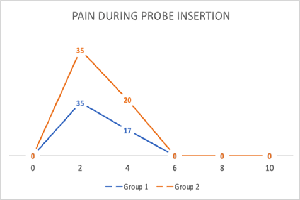
Background: Transrectal ultrasound-guided prostate biopsy (TRUS PBx) is a widely used method for diagnosing prostate cancer. Ensuring effective pain control during this procedure is essential for patient comfort and compliance. Apical periprostatic nerve block (PNB) and intrarectal topical anaesthesia (ITA) are two commonly employed anaesthetic techniques. This study aimed to compare the analgesic effectiveness of apical PNB versus ITA during TRUS-guided prostate biopsy. Methods: In this prospective, randomised comparative trial, participants were allocated into two groups. Group 1 was administered 10ml of 2% lignocaine through apical periprostatic infiltration, whereas Group 2 received 10ml of xylocaine gel via intrarectal application. Pain assessment was performed using the Wong-Baker FACES Pain Rating Scale (WBFPRS) during probe insertion, biopsy, and post-procedure. Baseline characteristics were comparable between groups. Results: Both anaesthetic techniques relieved pain; however, Group 1 consistently exhibited lower pain scores. During biopsy, Group 1 reported significantly less pain than Group 2 (p = 0.001), and this difference remained significant 30 minutes post-procedure (p = 0.001). Most patients in Group 1 recorded pain scores of 0 or 2 post-biopsy, indicating minimal discomfort. On Day 3 follow-up, no significant differences were observed in post-biopsy complications, although there was a non-significant trend toward increased haematuria in the ITA group (p = 0.304). Conclusion: Apical PNB is more effective than ITA for pain control during TRUS PBx and does not influence delayed post-procedural outcomes. These results support the efficacy of apical periprostatic nerve block (PNB) in improving patient comfort during prostate biopsy, without compromising procedural safety.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dr Dron Sharma, Dr Puvvada Sandeep, Dr Prasad Mylarappa, Dr Manasa T

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Bingqian L, Peihuan L, Yudong W, Jinxing W, Zhiyong W. Intraprostatic local anaesthesia with periprostatic nerve block for transrectal ultrasound-guided prostate biopsy. J Urol. 2014;182:479–83.
[2] Guo G, Xu Y, Zhang X. TRUS guided transperineal prostate 12+X core biopsy with template for the diagnosis of prostate cancer. Oncol Lett 2017;13:4863 7.
[3] Saraçoğlu T, Unsal A, Taşkın F, Sevinçok L, Karaman CZ. The impact of pre-procedural waiting period & anxiety level on pain perception in patients undergoing transrectal ultrasound-guided prostate biopsy. Diagn Interv Radiol. 2013;18:195–9.
[4] Ochiai A, Babaian RJ. Update on prostate biopsy technique. Curr Opin Urol. 2014;14:157–62.
[5] Cevik I, Ozveri H, Dillioglugil O, Akdaş A. Lack of effect of intrarectal lidocaine for pain control during transrectal prostate biopsy: A randomised prospective study. Eur Urol 2012;42:217‑20.
[6] Alabi TO, Tijani KH, Adeyomoye AA, Jeje EA, Anunobi CC, Ogunjimi MA, et al. Combined intrarectal lidocaine gel & periprostatic nerve block: A ‘balanced’ anaesthesia for transrectal ultrasound guided prostate biopsy? Niger Postgrad Med J 2018;25:252 6.
[7] Yang Y, Liu Z, Wei Q, Cao D, Yang L, Zhu Y, et al. The efficiency & safety of intra-rectal topical anaesthesia for transrectal ultrasound guided prostate biopsy: A systematic review & meta-analysis. Urol Int 2017;99:373 83.
[8] Gurbuz C, Canat L, Bayram G, Gokhan A, Samet G, Caskurlu T. Visual pain score during transrectal ultrasound‑guided prostate biopsy using no anaesthesia or three different types of local anaesthetic application. Scand J Urol Nephrol 2016;44:212‑6.
[9] Song SH, Kim JK, Song K, Ahn H, Kim CS. Effectiveness of local anaesthesia techniques in patients undergoing transrectal ultrasound‑guided prostate biopsy: A prospective randomised study. Int J Urol 2016;13:707‑10.
[10] Madej A, Wilkosz J, Różański W, Lipiński M. Complication rates after prostate biopsy according to the number of sampled cores. Cent European J Urol 2012;65:116 8.
[11] Wang J, Wang L, Du Y, He D, Chen X, Li L, et al. Addition of intrarectal local analgesia to periprostatic nerve block improves pain control for transrectal ultrasonography-guided prostate biopsy: A systematic review and meta-analysis. Int J Urol 2015;22:62 8.
[12] Ozah E, Ezenwa EV, Agbugui JO, Osaigbovo EO. Transrectal ultrasound-guided prostate biopsy in University of Benin teaching hospital: effect of prostate volume on pain amongst Nigerian patients. Am J Clin Exp Urol. 2021 Feb 15;9(1):157-162.
[13] Moinzadeh A, Mourtzinos A, Triaca V, Hamawy KJ. A randomised double blind prospective study evaluating patient tolerance of transrectal ultrasound-guided biopsy of the prostate using prebiopsy rofecoxib. Urology 2013;62:1054 7.
[14] Maccagnano C, Scattoni V, Roscigno M, Raber M, Angiolilli D, Montorsi F, et al. Anaesthesia in transrectal prostate biopsy: Which is the most effective technique? Urol Int 2011;87:1 13.