Aplastic Anemia in Southern Odisha: An Institutional Study of Clinical and Hematological Features
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
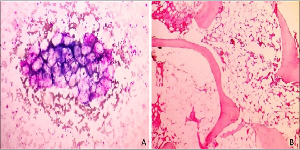
Introduction: Aplastic anemia is a potentially life-threatening failure of hematopoiesis, characterized by pancytopenia and hypocellular bone marrow. Aplastic anemia if untreated results in very high mortality. Early diagnosis of aplastic anemias is essential for appropriate management of the patient. Aims and Objectives: The aim of the study was to assess the prevalence of the condition in southern Odisha admitted to this institute and to study the clinico-hematological profile for the assessment of severity by using the modified Camitta criteria aiding in their management protocol. Materials and Methods: This study was carried out prospectively in the Department of Pathology, MKCG Medical College & Hospital during the period of June 2017 to May 2019. A detailed clinical history, physical examination, Complete Blood Count, CPS, Reticulocyte count, Bone marrow aspiration and Biopsy were performed in each case and the observations were evaluated using simple and basic statistical tools. Results: There are 63 diagnosed cases of aplastic anemia during the study period. Out of 63 cases 36 cases are male (57.1%) and 27 cases are female (42.8 %) indicating a male preponderance of this disease and male to female ratio is1.3:1. We also found that, aplastic anemia has a bimodal age distribution. Fever, generalized weakness and bleeding due to thrombocytopenia are commonest clinical manifestations. All 63 cases are subcategorized into 38 Non severe cases (60.3%), 17 severe cases (26.9%) and 8 cases are very severe (12.7 %). Conclusion: A good knowledge on clinical and hematological parameters will certainly aid in early diagnosis of aplastic anemia and sub-categorization for treatment. But in a developing country financial constraints and lack of awareness forms a major drawback in patient management. So early diagnosis of aplastic anemia reduces the treatment cost as well as will decrease mortality.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Binaya Bhusan Bihari, Atanu Kumar Bal, Shushruta Mohanty, Devidutta Ramani Ranjan Rout, Sashibhusan Dash

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Sashibhusan Dash, Multidisciplinary Research Unit, Pandit Raghunath Murmu Medical College & Hospital, Baripada, Odisha, India.
Corresponding author: Dr. Atanu Kumar Bal
Multidisciplinary Research Unit, Pandit Raghunath Murmu Medical College & Hospital, Baripada, Odisha, India.
[1] Schoettler ML, Nathan DG. The Pathophysiology of Acquired Aplastic Anemia: Current Concepts Revisited. Hematol Oncol Clin North Am. 2018 Aug; 32(4):581-594.
[2] Jha SC, Singh A, Mazuffar MA et al. Acquired idiopathic aplastic anemia; Study of 20 cases and review of literature. Inter J Bio Adv Res.2015; 6:569-73.
[3] Furlong E, Carter T. Aplastic anaemia: Current concepts in diagnosis and management. J Paediatr Child Health. 2020;56(7):1023-1028.
[4] Montané E, Ibáñez L, Vidal X, et al. Epidemiology of aplastic anemia: a prospective multicenter study. Haematologica. 2008; 93(4):518-523.
[5] Ahmed P, Chaudhry QUN, Satti TM, et al. Epidemiology of aplastic anemia: a study of 1324 cases. Hematology. 2020;25(1):48-54.
[6] Issaragrisil S, Kaufman DW, Anderson T, et al. The epidemiology of aplastic anemia in Thailand. Blood. 2006; 107(4):1299-1307.
[7] McCahon E, Tang K, Rogers PC, McBride ML, Schultz KR. The impact of Asian descent on the incidence of acquired severe aplastic anaemia in children. Br J Haematol. 2003; 121(1):170-172.
[8] Mahapatra M, Singh PK, Agarwal M, et al. Epidemiology, Clinico-Haematological Profile and Management of Aplastic Anaemia: AIIMS Experience. J Assoc Physicians India. 2015;63(3 Suppl):30-35.
[9] Gupta V, Kumar A, Saini I, Saxena AK. Cytogenetic profile of aplastic anaemia in Indian children. Indian J Med Res. 2013; 137(3):502-506.
[10] Aziz T, Ali L, Ansari T, Liaquat HB, Shah S, Ara J. Pancytopenia: megaloblastic anemia is still the commonest cause. Pak J Med Sci. 20101; 26(1):132-6.
[11] Naseem S, Varma N, Das R, Ahluwalia J, Sachdeva MU, Marwaha RK. Pediatric patients with bicytopenia/pancytopenia: review of etiologies and clinico-hematological profile at a tertiary center. Indian J Pathol Microbiol. 2011; 54(1):75-80.
[12] Gayathri BN, Rao KS. Pancytopenia: a clinico hematological study. J Lab Physicians. 2011 Jan;3(1):15-20.
[13] Vaht K, Göransson M, Carlson K, et al. Incidence and outcome of acquired aplastic anemia: real-world data from patients diagnosed in Sweden from 2000-2011. Haematologica. 2017 Oct;102(10):1683-1690.
[14] Bain BJ. Bone marrow trephine biopsy. J Clin Pathol. 2001;54(10):737-742.
[15] Bulduk T. Aplastic anemia from past to the present: A bibliometric analysis with research trends and global productivity during 1980 to 2022. Medicine (Baltimore). 2023;102(36): e34862.
[16] Parapia LA. Trepanning or trephines: a history of bone marrow biopsy. Br J Haematol. 2007;139(1):14-19.