Fetal Hemoglobin (HbF) as a Genetic Modulator in Various Clinical Phenotypes of Sickle Cell Anemia in Tribal and Non-Tribal Ethnic Group of Saurashtra Region in Gujarat
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
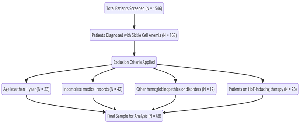
Objectives: To compare fetal hemoglobin (HbF) levels and clinical manifestations between Tribal and non-Tribal Sickle Cell Anemia (SCA) patients in Gujarat's Saurashtra region and investigate HbF's role in modulating disease severity. Methods: This retrospective study analyzed 68 SCA patients (33 Tribal, 35 non-Tribal) at a tertiary care center from January 2023-2024. HbF levels were measured via high-performance liquid chromatography, and clinical data on Acute Chest Syndrome (ACS), Vaso-occlusive Events (VOE), Pain Crisis, and hospitalization duration were collected from medical records. Results: Tribal patients exhibited significantly higher mean HbF levels compared to non-Tribal patients (17.8% vs. 13.0%, p<0.01). This correlated with lower incidence of ACS (36% vs. 65%, p=0.0176) and VOE (39% vs. 77%, p=0.0016) among Tribal patients. Pain Crisis incidence showed no significant difference between groups (36% vs. 45%, p=0.4535). Notably, Tribal patients experienced shorter mean hospital stays (2.12 vs. 3.37 days, p<0.01). Conclusion: Higher HbF levels in Tribal SCA patients correlate with reduced ACS and VOE incidence and shorter hospitalizations, suggesting a protective effect. These findings enhance understanding of SCA heterogeneity across ethnic groups and may inform development of population-specific management approaches. Further investigation into genetic and environmental factors underlying these differences is warranted.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dhara P Trivedi, Deval Mehta, Punithan Narayanan, Pragati Kantibhai Bhimani

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Deval Mehta, Tutor, Department of Pathology, Shri M P Shah Medical College, Jamnagar, Gujarat, India.
Tutor, Department of Pathology, Shri M P Shah Medical College, Jamnagar, Gujarat, India.
[1] Piel, F. B., Patil, A. P., Howes, R. E., Nyangiri, O. A., Gething, P. W., Williams, T. N., ... & Hay, S. I. (2013). Global distribution of the sickle cell gene and geographical confirmation of the malaria hypothesis. Nature Communications, 4(1), 1-9.
[2] Colah, R. B., Mukherjee, M. B., Martin, S., & Ghosh, K. (2015). Sickle cell disease in tribal populations in India. Indian Journal of Medical Research, 141(5), 509-515.
[3] Rees, D. C., Williams, T. N., & Gladwin, M. T. (2010). Sickle-cell disease. The Lancet, 376(9757), 2018-2031.
[4] Steinberg, M. H., Chui, D. H., Dover, G. J., Sebastiani, P., & Alsultan, A. (2014). Fetal hemoglobin in sickle cell anemia: a glass half full? Blood, 123(4), 481-485.
[5] Akinsheye, I., Alsultan, A., Solovieff, N., Ngo, D., Baldwin, C. T., Sebastiani, P., ... & Steinberg, M. H. (2011). Fetal hemoglobin in sickle cell anemia. Blood, 118(1), 19-27.
[6] Platt, O. S., Brambilla, D. J., Rosse, W. F., Milner, P. F., Castro, O., Steinberg, M. H., & Klug, P. P. (1994). Mortality in sickle cell disease--life expectancy and risk factors for early death. New England Journal of Medicine, 330(23), 1639-1644.
[7] Alsultan, A., Alabdulaali, M. K., Griffin, P. J., AlSuliman, A. M., Ghabbour, H. A., Sebastiani, P., ... & Steinberg, M. H. (2014). Sickle cell disease in Saudi Arabia: the phenotype in adults with the Arab-Indian haplotype is not benign. British Journal of Haematology, 164(4), 597-604.
[8] Kar, B. C., Satapathy, R. K., Kulozik, A. E., Kulozik, M., Sirr, S., Serjeant, B. E., & Serjeant, G. R. (2014). Sickle cell disease in Orissa State, India. The Lancet, 2(8327), 1198-1201.
[9] Piel, F. B., Patil, A. P., Howes, R. E., Nyangiri, O. A., Gething, P. W., Williams, T. N., ... & Hay, S. I. (2013). Global distribution of the sickle cell gene and geographical confirmation of the malaria hypothesis. Nature Communications, 4(1), 1-9.
[10] Meier, E. R., Fasano, R. M., & Levett, P. R. (2017). A systematic review of the literature for severity predictors in children with sickle cell anemia. Blood Cells, Molecules, and Diseases, 65, 86-94.
[11] Chakravorty, S., & Williams, T. N. (2015). Sickle cell disease: A neglected chronic disease of increasing global health importance. Archives of Disease in Childhood, 100(1), 48-53.