An Observational Study on Success of Ureteral Access Sheath Placement during Primary Retrograde Intra-Renal Surgery for Renal Stones
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
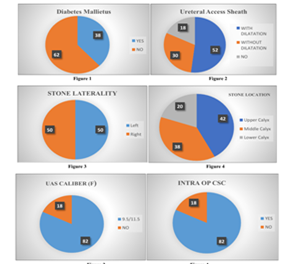
Background: This study explores the effectiveness and challenges of ureteral access sheath (UAS) placement during retrograde intrarenal surgery (RIRS) for treating renal stones. This study aims to evaluate the success of ureteral access sheath (UAS) placement during primary retrograde intrarenal surgery (RIRS) for renal stones, with a focus on assessing both placement success and related complications and stone-free rates. Methods: This cross-sectional observational study was conducted over six months at M S Ramaiah Medical College, Bengaluru, India, focusing on patients aged 21 to 80 years with renal stones measuring 10 mm to 20 mm. The study evaluated UAS placement success, intraoperative stone-free rates. Data collection included demographics, stone characteristics, and surgical parameters. Statistical analysis employed descriptive and inferential methods. Results: Among 50 patients (52% female, 48% male), diabetes mellitus was present in 38%. Stones were primarily located in the upper calyx (42%). The UAS was utilized in 82% of cases, with 52% requiring dilatation. Intraoperative complete stone clearance occurred in 82% of procedures, and total intraoperative time was significantly prolonged in cases of complete stone clearance (p < 0.001). Conclusion: The study highlights the challenges of UAS placement in RIRS for renal stones in Indian patients, particularly concerning larger stone burdens and abnormal ureteral anatomy. Future approaches should focus on individualized strategies to optimize surgical outcomes and reduce complications.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dr Dron Sharma, Dr Shashwat Singh, Dr M A Vivek Kumar, Dr Rajat Agarwal, Dr Rakesh Patil, Dr Mahesh Chalumuru, Dr D Ramesh, Dr Tarun Javali, Dr Puvvada Sandeep

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Bultitude M, Smith D, Thomas K. Contemporary Management of Stone Disease: The New EAU Urolithiasis Guidelines for 2015. Eur Urol 2016;69:483-4.
[2] Breda A, Emiliani E, Millan F, et al. The new concept of ureteral access sheath with guidewire disengagement: One wire does it all. World J Urol 2016;34:603-6.
[3] Oktay Özman, Hacı M. Akgül, Cem Başataç, Multi-aspect analysis of ureteral access sheath usage in retrograde intrarenal surgery: A RIRSearch group study, Asian Journal of Urology, Volume 11, Issue 1, 2024, Pages 80-85, ISSN 2214-3882
[4] De Coninck V, Somani B, Sener ET, Emiliani E,. Ureteral Access Sheaths and Its Use in the Future: A Comprehensive Update Based on a Literature Review. J Clin Med. 2022 Aug 31;11(17):5128. doi: 10.3390/jcm11175128. PMID: 36079058; PMCID: PMC9456781.
[5] De Coninck V., Keller E.X., Rodriguez-Monsalve M., Audouin M., Doizi S., Traxer O. Systematic review of ureteral access sheaths: Facts and myths. BJU Int. 2018; 122:959-969. doi: 10.1111/bju.14389
[6] Huang J., Zhao Z., AlSmadi J.K., Liang X. Use of the ureteral access sheath during ureteroscopy: A systematic review and meta-analysis. PLoS ONE. 2018;13:e0193600. doi: 10.1371/journal.pone.0193600.
[7] Agrawal S., Patil A., Sabnis R.B., Singh A.G., Ganpule A.P., Desai M.R. Initial experience with slimmest single-use flexible ureteroscope Uscope PU3033A (PUSEN) in retrograde intrarenal surgery and its comparison with Uscope PU3022a: A single-center prospective study. World J. Urol. 2021;39:3957-3962.
[8] Shrestha A., Gharti B.B., Adhikari B. Perirenal Extravasation After Retrograde Intrarenal Surgery for Renal Stones: A Prospective Study. Cureus. 2022;14:e21283. doi: 10.7759/cureus.21283
[9] Damar E., Senocak C., Ozbek R., Haberal H.B., Sadioglu F.E., Yordam M., Bozkurt O.F. Does ureteral access sheath affect the outcomes of retrograde intrarenal surgery: A prospective study. Minim. Invasive Ther. Allied Technol. 2021;31:777-781
[10] Lima A., Reeves T., Geraghty R., Pietropaolo A., Whitehurst L., Somani B.K. Impact of ureteral access sheath on renal stone treatment: Prospective comparative non-randomised outcomes over a 7-year period. World J. Urol. 2020;38:1329-1333
[11] Yuk, H.D., Park, J., Cho, S.Y. et al. The effect of preoperative ureteral stenting in retrograde Intrarenal surgery: a multicenter, propensity score-matched study. BMC Urol 20, 147 (2020).
[12] Kaplan AG, Lipkin ME, Scales CD Jr, et al. Use of ureteral access sheaths in ureteroscopy. Nat Rev Urol 2016;13:135-40.