Newer Trends of Photodermatoses in Patients Attending Dermatology OPD in a Tertiary Care Center in Rural South India: An Observational Study
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
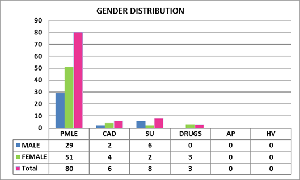
Background: Photodermatoses are skin conditions caused by electromagnetic radiation, which can come from artificial or solar sources including UV, visible light, and infrared (IR) radiation. Methods: Our study was conducted in a tertiary care center of Palakkad district in Kerala which is the gateway to Kerala due to the presence of the Palakkad Gap in the Western Ghats. Palakkad has a tropical wet and dry climate. The district being granary of Kerala, farming is a major occupation. According to Lehmann and Schwarz, photodermatoses can affect a person's quality of life but are not life-threatening, so prevention is more crucial. A descriptive cross-sectional study was designed and conducted for 1 year during February 2023 to January 2024. Results: A total of 97 patients with photodermatoses attended our OPD during the study period Prevalence was calculated to be 0.54%. Majority of the patients presented as PMLE (82%) as papules (47%) involving the upper limb (54%). Maximum cases had onset in the month of April, May and June. Conclusion: Manual labourers and Farmers who are exposed to direct sunlight >6 hours have high risk of developing photodermatoses. Photodermatoses are skin disorders mostly influenced by the age, socioeconomic status, and occupation of the patients. Standard operations protocol has to be implemented by state labour department regarding work hours of manual labourers with a mandatory 3 hours break in the afternoon from 12pm to 3pm and strict measures to ensure adherence with the same.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Prathyusha Prabhakar, Darsan S, Rudra Priya S

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] M. Bylaite, J. Grigaitiene, G.S. Lapinskaite. Photodermatoses: classification, evaluation and management. Br J Dermatol, 161 (2009), pp. 61-68.
[2] Lehmann P, Schwarz T. Photodermatoses: diagnosis and treatment. Deutsches Ärzteblatt International. 2011 Mar;108(9):13.
[3] R. Roelandts. Photodermatology. Quo vadis?. Actas Dermosifiliogr, 100 (2009), pp. 66-72.
[4] Yashar SS, Lim HW. Classification and evaluation of photodermatoses. Dermatologic therapy. 2003 Mar;16 (1):1-7.
[5] Mehta RV, Shenoi SD, Balachandran C, Pai S. Minimal erythema response (MED) to solar simulated irradiation in normal Indian skin. Indian J Dermatol Venereol Leprol. 2004;70(5):277-79.
[6] Sharma VK, Sahni K, Wadhwani AR. Photodermatoses in pigmented skin. Photochem Photobiol Sci. 2013;12(1):65-77.
[7] Srinivas CR, Sekar CS, Jayashree R. Photodermatoses in India. Indian DermatolVenereol Leprol. 2012;78, Suppl S1:01-08.
[8] Sahoo BS, Panda S, Pati S, Sabat SK. Clinical and Epidemiological Profile of Idiopathic Photodermatoses: A Study in a Tertiary Care Setting. European Journal of Cardiovascular Medicine. 2023 Oct 1;13(4).
[9] Nagaraju GV, Haranath PV, Rahaman K, Pranadeep NT, Kumar GP, Parvathi NS. Evalution of clinical spectrum and frequency of photodermatoses in a skin speciality hospital. IAJPR. 2018;8(6):1378-89.
[10] Sharma L, Basnet A. A clinicoepidemiological study of polymorphic light eruption. 2008.
[11] Wadhwani AR, Sharma VK, Ramam M, Khaitan BK. A clinical study of the spectrum of photodermatoses in dark-skinned populations. Clin Exp Dermatol. 2013 Dec;38(8):823-9. doi: 10.1111/ced.12098. Epub 2013 Jun 13. PMID: 23758593.
[12] Verma K, Rokde R, Singh U. A clinic epidemiological and histo-pathological study of polymorphic light eruptions in malwa region. Indian J Clin Exp Dermatol. 2019; 5:24-9.
[13] Deshmukh AR, Pathrikar SS, Khedkar MY, Mahajan KR, Sherasiya BS. Clinic epidemiological study of polymorphous light eruption in Marathwada region. Int J Recent trends Sci Technol.2015; 17:128-30.
[14] Sharma P, Shah A, Lachhiramani R, Jagati A. Spectrum of dermatological manifestation in all female attending tertiary health care in a developing country. Int J Med Res Rev 2018; 6(08): 420-426.