Exploring Laboratory Errors in Blood Transfusion: A Systematic Review
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
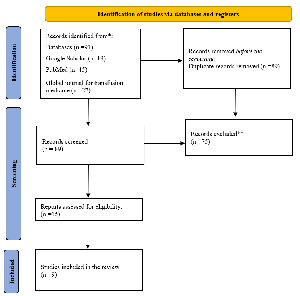
Blood transfusion, a vital medical intervention, is susceptible to errors in the laboratory phase, which can lead to severe consequences. This systematic review explores the literature on laboratory errors in blood transfusion, highlighting the impact of these errors on patient safety and outcomes. It also presents strategies for error prevention and management. The review underscores the potential for improvement in blood transfusion services through ongoing quality improvement efforts, a responsibility for all of us. After a comprehensive search and analysis of relevant literature published from 2014 to 2024 under PARSMA2020 guidelines, nine articles met the inclusion criteria, revealing a range of errors across different stages of the transfusion process. Preanalytical errors were found to be the most common. Procedural deviations, insufficient collaboration, and work fatigue among medical staff were identified as the causes of these errors. The review suggests that implementing educational and contentious training programs for medical staff, along with highly accountable policies, could significantly reduce these errors, thereby reducing total mortality and morbidity rates.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2024 Samah Gamar Aldeen Abdelhadi Mahmoud, Abdalla Eltoum Ali, Al-Neil M. Hamza

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Abdollahi, A., Saffar, H., & Saffar, H. (2014). Types and Frequency of Errors during Different Phases of Testing at a Clinical Medical Laboratory of a Teaching Hospital in Tehran, Iran. North American journal of medical sciences, 224-228.
AL-ESHAQ, D. H., (2020). The Use of Data-driven Quality Strategy to Improve the Processes of Patient Identification and Pre-transfusion Specimen Collection Documentation at Sidra Medicine. qu.edu.qa
Andriessen, J.W., Breard, M., Briggs, L., Butch, S., Distler, P., Georgsen, J., Goudar, S., Laakso, T. and Nozick, R., 2022. International Society for Blood Transfusion Guidelines for Validation of Automated Systems in Blood Establishments. Vox Sanguinis, 117(12), pp.1420-1445. Du. Dk
Antoniadi, A.M., Du, Y., Guendouz, Y., Wei, L., Mazo, C., Becker, B.A. & Mooney, C. (2021). Current challenges and future opportunities for XAI in machine learning-based clinical decision support systems: a systematic review. Applied Sciences, 11(11), 5088. mdpi.com
Badrick, T., (2021). Integrating quality control and external quality assurance. Clinical biochemistry. [HTML]
Bolton‐Maggs, P. H. B. & Watt, A., (2020). Transfusion errors—can they be eliminated? British journal of hematology. [HTML]
Bolton-Maggs, P., & Cohen, H. (2013). Serious Hazards of Transfusion (SHOT) haemovigilance and progress is improving transfusion safety. British Journal of Haematology, 303–314.
Brown, C. & Brown, M., (2023). Blood and blood products transfusion errors: What can we do to improve patient safety? British Journal of Nursing. [HTML]
Cagliano, A.C., Grimaldi, S. and Rafele, C., 2021. A structured approach to analyze logistics risks in the blood transfusion process. Journal of Healthcare Risk Management, 41(2), pp.18-30. [HTML]
Dandekar, A., Save, S., Bhandarkar, S., Desai, M., Shah, J., Lapsia, P., Bhagat, M., Zinjal, R., Shah, P., Shital, N. and Hakhu, S., 2021. Pre-transfusion Blood Testing Device. In Advances in Medical Physics and Healthcare Engineering: Proceedings of AMPHE 2020 (pp. 247-253). Springer Singapore. researchgate.net
Fernandes, M., Vieira, S.M., Leite, F., Palos, C., Finkelstein, S. and Sousa, J.M., 2020. Clinical decision support systems for triage in the emergency department using intelligent systems: a review. Artificial Intelligence in Medicine, 102, p.101762. e-tarjome.com
Howard, P. R. (2020). … & Applied Concepts of Blood Banking and Transfusion Practices-E-Book: Basic & Applied Concepts of Blood Banking and Transfusion Practices-E-Book. [HTML]
Iwen, P.C., Stiles, K.L. and Pentella, M.A., (2020). Safety considerations in the laboratory testing of specimens suspected or known to contain the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). American Journal of Clinical Pathology, 153(5), 567–570. nih.gov
Kau, G., Kaur, G., & Kaur, P. (2019). Nature and causes of errors in the blood transfusion chain– a step towards patient safety. International Society of Blood Transfusion, 193-200.
Lancaster, E.A., Rhodus, E.K., Duke, M.B. & Harris, A.M. (2021). Blood transfusion errors within a health system: A review of root cause analyses. Patient Safety, 3(2), 78–91. scholasticahq.com
Mascotti, K. M., 2021. Quality Programs in Blood Banking and Transfusion Medicine. Transfusion Medicine. [HTML]
Moiz, B., Siddiqui, A.K., Sana, N., Sadiq, M.W., Karim, F. and Ali, N., 2020. Documentation errors in transfusion chain: Challenges and interventions. Transfusion and Apheresis Science, 59(4), p.102812. gciamt.org
Nichols, J.H., Alter, D., Chen, Y., Isbell, T.S., Jacobs, E., Moore, N. & Shajani-Yi, Z. (2020). AACC guidance document on management of point-of-care testing. The Journal of Applied Laboratory Medicine, 5(4), 762–787. myadlm.org
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372: n71. doi: 10.1136/bmj. n71. http://www.prisma-statement.org/
Padalko, E., Colenbie, L., Delforge, A., Ectors, N., Guns, J., Imbert, R., Jansens, H., Pirnay, J.P., Rodenbach, M.P., Van Riet, I. and Vansteenbrugge, A., 2023. Preanalytical variables influencing the interpretation and reporting of biological tests on blood samples of living and deceased donors for human body materials. Cell and Tissue Banking, pp.1-12. springer.com
Rambiritch, V., Vermeulen, M., Bell, H., Knox, P., Nedelcu, E., Al‐Riyami, A.Z., Callum, J., van den Berg, K. and Education Subcommittee of the AABB Global Transfusion Forum, 2021. Transfusion medicine and blood banking education and training for blood establishment laboratory staff: A review of selected African countries. Transfusion, 61(6), pp.1955-1965. nih.gov
Rambo, C. A. M. & Magnago, T. S. B. S., 2023. Construction and validity of checklist for patient safety during the transfusion process. Texto & Contexto-Enfermagem. scielo.br
Ri, M., Kasai, M., Kohno, A., Kondo, M., Sawa, M., Kinoshita, T., . . . Kato, H. (2020). A survey of blood transfusion errors in Aichi Prefecture in Japan: Identifying significant lapses threatening the safety of transfusion recipients: transfusion and Apheresis Science.
Sahmoud, S., Ashry, E.M., El Kalioby, M. and Kamel, N., 2021. Knowledge improvement of blood transfusion safety among pediatricians: post educational intervention. Transfusion Medicine Reviews, 35(2), pp.135-139. gciamt.org
Shahshahani, H. J., & Hayati, A. (2020). International Journal of Hematology-Oncology and Stem Cell Research Center. International Journal of Hematology-Oncology and Stem Cell Research, 38-44.
Sepetiene, R., Patamsyte, V., Robbins, N.F., Ali, M. and Carterson, A., (2021). The preanalytical phase for transfusion medicine and blood bank laboratory tasks are to be completed. Open Access Research Journal of Science and Technology, 3(1), 063–069. oarjst.com
Soliman, H.M. and Elhapashy, H.M., (2021). Nurses' Competence in Safety Blood Transfusion: The Impact of a Training Module. International Journal of Nursing Education, 13(3). researchgate.net
Strauss, R., Downie, H., Wilson, A., Mounchili, A., Berry, B., Cserti-Gazdewich, C., & Callum, J. (2018). Sample collection and sample handling errors submitted to the transfusion error surveillance system, 2006 to 2015. TRANSFUSION, 1697–1707.
Das, S. S., Chakrabarty, R., & Zaman, R. (2017). Monitoring Errors in a Blood Bank Immunohematology Laboratory: Implementing Strategies for Safe Blood Transfusion. Global Journal of Transfusion Medicine, 118-123.
Jain, A., Kumari, S., Marwaha, N., & Sharma, R. R. (2014). The Role of Comprehensive Check at the Blood Bank Reception on Blood Requisitions Detecting Potential Transfusion Errors. Indian Society of Haematology & Transfusion Medicine, 269–274.
Makroo, R. N., & Bhatia, A. (2017). Delta checks for blood groups: A step ahead in blood safety. 7 Asian Journal of Transfusion Science, 18-21.
Miah, S. S., Doha, M. A., Islam, M., & Sharmin, N. (2021). The First Data of Hemovigilance: Appraised from a single center in Bangladesh. 1 Global Journal of Transfusion Medicine, pp. 218–223.
Vijenthira, S., Armali, C., Downie, H., Wilson, A., Paton, K., Berry, B., . . . Callum, J. (2021). Registration errors among patients receiving blood transfusions: a national analysis from 2008 to 2017. International Society of Blood Transfusion, 225–233.
Health Organization, W., 2021. Guidance on centralization of blood donation testing and processing. Who. Int
Yami, A., Darbandi, A., Saber, E., Tabrizi Namini, M. and Gharehbaghian, A., 2021. Assessment of the knowledge of blood transfusion in Iranian nurses of Tehran's hospitals. Transfusion Medicine, 31(6), pp.459-466. researchgate.net