Rest or Burnout? Unveiling the Link Between Sleep Quality and Life Satisfaction in Resident Doctors: A Cross-Sectional Study
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
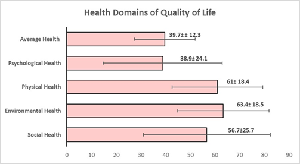
Background: Long and irregular duty hours impair sleep quality in resident doctors, affecting their quality of life (QoL) and increasing health risks. This study explores the relationship between sleep quality and QoL to promote their well-being. Methods: A cross-sectional study was conducted among 50 medical residents (23–45 years) after ethical approval and consent. Sleep quality was assessed using the Pittsburgh Sleep Quality Index and Quality of Life using the WHO Quality of Life-BREF questionnaire. Data were analyzed using means, standard deviations, and proportions, with p<0.05 as significant. Results: Overall Quality of Life was high in 80% of participants (mean score: 4.28 ± 0.829). Sleep impairment was moderate (PSQI: 8.6 ± 2.626). Environmental (63.4 ± 18.5), physical (61.0 ± 18.4), and social health (56.7 ± 25.7) domains showed moderate well-being, whereas psychological (38.9 ± 24.1) and general health (39.7 ± 12.3) were lower, indicating mental health concerns. A moderate negative correlation (R² = 0.117) was found between sleep quality and QoL. Conclusion: Poor sleep quality and psychological distress are prevalent among resident doctors, highlighting the need for interventions to improve sleep and mental well-being.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Jitendra Singh, Anuradha Yadav, PhD, Sandeep Saxena

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Defoe DM, Power ML, Holzman GB, Carpentieri A, Schulkin J. Long hours and little sleep: work schedules of residents in obstetrics and gynecology. Obstet Gynecol. 2001 Jun;97(6):1015-8. doi: 10.1016/s0029-7844(01)01363-1. PMID: 11384712.
[2] Pega F, Náfrádi B, Momen NC, Ujita Y, Streicher KN, Prüss-Üstün AM; Technical Advisory Group; Descatha A, Driscoll T, Fischer FM, Godderis L, Kiiver HM, Li J, Magnusson Hanson LL, Rugulies R, Sørensen K, Woodruff TJ. Global, regional, and national burdens of ischemic heart disease and stroke attributable to exposure to long working hours for 194 countries, 2000-2016: A systematic analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Environ Int. 2021 Sep;154:106595. doi: 10.1016/j.envint.2021.106595. Epub 2021 May 17. PMID: 34011457; PMCID: PMC8204267.
[3] Dey R, Dutta S, Bhandari SS. Sleep Quality and Daytime Sleepiness among the Clinicians Working in a Tertiary Care Center in Sikkim, India. Indian J Psychol Med. 2020 Mar 9;42(2):141-146. doi: 10.4103/IJPSYM.IJPSYM_439_18. PMID: 32346255; PMCID: PMC7173663.
[4] Kelly MM, Brace M. Cardiovascular risk emerges earlier by birth weight and preterm birth status in the United States Add Health sample. Int J Cardiol. 2025 Mar 15;423:132994. doi: 10.1016/j.ijcard.2025.132994. Epub 2025 Jan 18. PMID: 39832537.
[5] Rivera AS, Akanbi M, O’Dwyer LC, McHugh M. Shift work and long work hours and their association with chronic health conditions: A systematic review of systematic reviews with meta-analyses. Beiki O, editor. PLOS ONE. 2020 Apr 2;15(4). https://doi.org/10.1371/journal.pone.0231037.
[6] Bøggild H, Knutsson A. Shift work, risk factors and cardiovascular disease. Scand J Work Environ Health. 1999 Apr;25(2):85-99. doi: 10.5271/sjweh.410. PMID: 10360463.
[7] Ju YS, Ooms SJ, Sutphen C, Macauley SL, Zangrilli MA, Jerome G, et al. Slow wave sleep disruption increases cerebrospinal fluid amyloid-β levels. Brain. 2017 Jul 10;140(8):2104-11. doi: 10.1093/brain/awx148. PMID: 28899014; PMCID: PMC5790144.
[8] Cunningham TR, Guerin RJ, Ferguson J, Cavallari J. Work-related fatigue: A hazard for workers experiencing disproportionate occupational risks. Am J Ind Med. 2022 Nov;65(11):913-925. doi: 10.1002/ajim.23325. Epub 2022 Jan 27. PMID: 35088430; PMCID: PMC9325913.
[9] Redinger J, Kabil E, Forkin KT, Kleiman AM, Dunn LK. Resting and Recharging: A Narrative Review of Strategies to Improve Sleep During Residency Training. J Grad Med Educ. 2022 Aug;14(4):420-430. doi: 10.4300/JGME-D-21-01035.1. PMID: 35991104; PMCID: PMC9380640
[10] Alotaibi AD, Alosaimi FM, Alajlan AA, Bin Abdulrahman KA. The relationship between sleep quality, stress, and academic performance among medical students. J Family Community Med. 2020 Jan-Apr;27(1):23-28. doi: 10.4103/jfcm.JFCM_132_19. Epub 2020 Jan 13. PMID: 32030075; PMCID: PMC6984036.
[11] Prasad B, Arora VM. Sleep and Wellness in Residency Embracing the Shift. JAMA Network Open. 2024;7(10):e2438294. doi:10.1001/jamanetworkopen.2024.38294
[12] Alami YZ, Ghanim BT, Zyoud SE. Epworth sleepiness scale in medical residents: quality of sleep and its relationship to quality of life. Journal of Occupational Medicine and Toxicology. 2018 Dec;13(1):1-9. https://doi.org/10.1186/s12995-018-0203-z]
[13] Buysse DJ, Reynolds III CF, Monk TH, Hoch CC, Yeager AL, Kupfer DJ. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI). Sleep. 1991 Jul 1;14(4):331-8.
[14] World Health Organization. WHOQOL-BREF: introduction, administration, scoring and generic version of the assessment: field trial version, December 1996. World Health Organization; 1996.
[15] Singh A, Singh N, Dixit S, Kaur S, Chellaiyan VG, Alfred J. Satisfaction with life among MBBS students and resident doctors of a tertiary hospital in South Delhi. Int J Community Med Public Health [Internet]. 2021 Nov. 24 [cited 2025 Apr. 5];8(12):5843-6. Available from: https://www.ijcmph.com/index.php/ijcmph/article/view/9035
[16] Chellaiyan DVG, Gupta S, Britto JJ, Kamble B. Job Satisfaction among Resident Doctors of a Tertiary Care Hospital in South Delhi. Indian J Occup Environ Med. 2022 Jul-Sep;26(3):151-156. doi: 10.4103/ijoem.ijoem_319_21. Epub 2022 Sep 26. PMID: 36408434; PMCID: PMC9674073.
[17] Fareeba, Rasheed Z, Saleema, Idrees A, Ahmad H, Sabir S, et al. An Evaluation of Work-Related Quality of Life Among General Surgery Residents Working in A Tertiary Care Hospital. Biological and Clinical Sciences Research Journal. 2024 Jun 20;2024(1):910–0.
[18] West CP, Dyrbye LN, Shanafelt TD. Physician burnout: Contributors, consequences, and solutions. J Intern Med. 2018;283(6):516-529.
[19] Dyrbye LN, West CP, Satele D, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2017;89(3):443-451.
[20] Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2019;172(18):1377-1385.
[21] A. Arr M, F. ALAhmadi A, A. Al-Harbi M, G. Al ghamdi A, A. Rahman Al-Dubai S. Quality of Life Among Physicians In Residency Programs In Al Madinah 2022. International Journal of Advanced Research. 2022 Apr 30;10(04):765–73. www.journalijar.com. https://doi.org/10.21474/ijar01/14614
[22] Mao Y, Raju G, Zabidi MA. Association Between Occupational Stress and Sleep Quality: A Systematic Review. Nat Sci Sleep. 2023 Nov 14;15:931-947. doi: 10.2147/NSS.S431442. PMID: 38021213; PMCID: PMC10656850.
[23] Walker MP. The Role of Sleep in Cognition and Emotion. Annals of the New York Academy of Sciences. 2009 Mar;1156(1):168–97. doi: 10.1111/j.1749-6632.2009.04416.x. PMID: 19338508.
[24] Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999 Oct 23;354(9188):1435-9. doi: 10.1016/S0140-6736(99)01376-8. PMID: 10543671.