Association Between Antibiotic Exposure and Type 2 Diabetes Risk: A Meta-Analysis
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
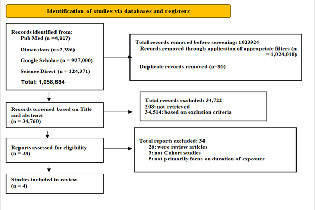
Type 2 diabetes mellitus (T2DM) is a significant contributor to morbidity and mortality globally and more than 500 million people are already affected. It has been estimated that almost 800 million may be living with T2DM by 2045. This review evaluated the association between antibiotic exposure and the risk of type 2 diabetes mellitus (T2DM). A systematic search of PubMed, Dimensions, Google Scholar and ScienceDirect was conducted on 5th June, 2025 and four (4) eligible studies were identified, that are all cohort studies. Data synthesis was performed using RevMan version 5.4.1, employing a fixed-effects model to pool hazard ratios (HR) with 95% confidence int ervals (CI). Heterogeneity and publication bias were assessed using I² statistics, Chi² tests, and funnel plots. The pooled HR identified was 1.31 (95% CI: 1.12–1.53), corresponding to a 31% increase in diabetes risk among individuals with longer antibiotic exposure compared to those unexposed. However, the overall effect was statistically significant (Z = 3.44, P < 0.0001). Moreover, substantial heterogeneity was observed across the four (4) studies (Chi² = 24.94, df = 3, P < 0.0001; I² = 88%). Ultimately, extended antibiotic duration and frequent/recurrent courses are each associated with increased risk of developing type 2 diabetes. Clinicians and patients should be aware of these potential long-term effects.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Olabisi Promise Lawal , Obiageri Ihuarulam Okeoma, Precious Esong Sone, Bolawa Fredrick Babatunde, Gabriel Dogbanya, Mary Tomi Olorunkosebi, Enikuomehin Oluwatoyin Justina

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Olabisi Promise Lawal , Department of Medical Laboratory Science, University of Benin, Benin City Nigeria.
Department of Medical Laboratory Science, University of Benin, Benin City Nigeria.
Obiageri Ihuarulam Okeoma, Department of Medical Laboratory Science, Trinity University Yaba, Lagos, Nigeria.
Department of Medical Laboratory Science, Trinity University Yaba, Lagos, Nigeria.
Precious Esong Sone, East Carolina University, Greenville, NC USA.
East Carolina University, Greenville, NC USA.
Bolawa Fredrick Babatunde, Department of Plant Science and Biotechnology, Adekunle Ajasin University, Akungba Akoko Ondo State Nigeria.
Department of Plant Science and Biotechnology, Adekunle Ajasin University, Akungba Akoko Ondo State Nigeria.
Gabriel Dogbanya, Department of Family Science, School of Public Health, University of Maryland College Park MD USA.
Department of Family Science, School of Public Health, University of Maryland College Park MD USA.
Mary Tomi Olorunkosebi, Department of Biological Sciences, Western Illinois University, Macomb, Illinois, USA.
Department of Biological Sciences, Western Illinois University, Macomb, Illinois, USA.
Enikuomehin Oluwatoyin Justina, Crimea Federal University, Ukraine.
Crimea Federal University, Ukraine.
[1] Hossain MJ, Al-Mamun M, Islam MR. Diabetes mellitus, the fastest growing global public health concern: Early detection should be focused. Health Sci Rep. 2024;7(3):e2004. doi:10.1002/hsr2.2004.
[2] Ahmed SK, Mohammed RA. Obesity: Prevalence, causes, consequences, management, preventive strategies and future research directions. Metab Open. 2025;27:100375. doi:10.1016/j.metop.2025.100375.
[3] Muteeb G, Rehman MT, Shahwan M, Aatif M. Origin of antibiotics and antibiotic resistance, and their impacts on drug development: A narrative review. Pharmaceuticals. 2023;16(11):1615. doi:10.3390/ph16111615.
[4] Hrncir T. Gut microbiota dysbiosis: Triggers, consequences, diagnostic and therapeutic options. Microorganisms. 2022;10(3):578. doi:10.3390/microorganisms10030578.
[5] Lawal OP, Adekunle JF, Abiodun AV, Orobator ET, Agbo OS, Ugoagwu KU, et al. Modulating gut microbiota for precision medicine in diabetes: a paradigm shift in personalized treatment strategies. Asian J Res Rep Endocrinol. 2025;8(1):94-109. doi:10.9734/ajrre/2025/v8i1110.
[6] Holt RIG, Cockram CS, Ma RCW, Luk AOY. Diabetes and infection: Review of the epidemiology, mechanisms and principles of treatment. Diabetologia. 2024;67(7):1168-80. doi:10.1007/s00125-024-06247-3.
[7] Li Z, He Q, He X, Xing X, Fu S, Sun X, et al. Long-term or recurrent antibiotic use in early life and the risk of type 2 diabetes: A population-based prospective cohort and a case–control study. J Diabetes. 2025;17(6):e70113. doi:10.1111/1753-0407.70113.
[8] Zacher M, Wedow R. Lessons in adjusting for genetic confounding in population research on education and health. SSM Popul Health. 2025;31:101834. doi:10.1016/j.ssmph.2025.101834.
[9] Amir-Behghadami M, Janati A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. 2020;37(6):387. doi:10.1136/emermed-2020-209567.
[10] Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2015;6(7):e1000097. doi:10.1371/journal.pmed.1000097.
[11] Alharbi A, Stevenson M. Refining Boolean queries to identify relevant studies for systematic review updates. J Am Med Inform Assoc. 2020;27(11):1658-66. doi:10.1093/jamia/ocaa148.
[12] Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
[13] Yuan J, Hu YJ, Zheng J, Kim JH, Sumerlin T, Chen Y, He Y, Zhang C, Tang J, Pan Y, Moore M. Long-term use of antibiotics and risk of type 2 diabetes in women: a prospective cohort study. Int J Epidemiol. 2020;49(5):1572-81. doi:10.1093/ije/dyaa122.
[14] Nuotio J, Niiranen T, Laitinen TT, Miller J, Sabin MA, Havulinna AS, Viikari JSA, Rönnemaa T, Hutri-Kähönen N, Laitinen TP, Tossavainen P, Salomaa V, Raitakari OT, Burgner DP, Juonala M. Use of antibiotics and risk of type 2 diabetes, overweight and obesity: the Cardiovascular Risk in Young Finns Study and the national FINRISK study. BMC Endocr Disord. 2022;22(1):284. doi:10.1186/s12902-022-01197-y.
[15] Park SJ, Park YJ, Chang J, Choi S, Lee G, Son JS, Kim KH, Oh YH, Park SM. Association between antibiotics use and diabetes incidence in a nationally representative retrospective cohort among Koreans. Sci Rep. 2021;11(1):21681. doi:10.1038/s41598-021-01125-5.
[16] Li Z, He Q, He X, Xing X, Fu S, Sun X, Ma M, Wang D, Mi N, Zhao J, Yuan J, Yang K. Long-Term or Recurrent Antibiotic Use in Early Life and the Risk of Type 2 Diabetes: A Population-Based Prospective Cohort and a Case-Control Study. J Diabetes. 2025;17(6):e70113. doi:10.1111/1753-0407.70113.
[17] Lau J, Ioannidis JP, Terrin N, Schmid CH, Olkin I. The case of the misleading funnel plot. BMJ. 2006;333(7568):597-600. doi:10.1136/bmj.333.7568.597.
[18] Boursi B, Mamtani R, Haynes K, Yang YX. The effect of past antibiotic exposure on diabetes risk. Eur J Endocrinol. 2015;172(6):639-48. doi:10.1530/EJE-14-1163.
[19] Mikkelsen KH, Knop FK, Frost M, Hallas J, Pottegård A. Use of Antibiotics and Risk of Type 2 Diabetes: A Population-Based Case-Control Study. J Clin Endocrinol Metab. 2015;100(10):3633-40. doi:10.1210/jc.2015-2696.
[20] Chu L, Su D, Wang H, Aili D, Yimingniyazi B, Jiang Q, Dai J. Association between Antibiotic Exposure and Type 2 Diabetes Mellitus in Middle-Aged and Older Adults. Nutrients. 2023;15(5):1290. doi:10.3390/nu15051290.