Clinical and Demographic Landscape of Schizophrenia in India: Findings from a Multicenter Real-World SCHIZO INDIA Study
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
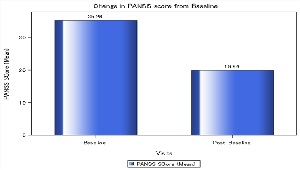
Background: The current real-world study aims to understand demographic details, clinical profiles, comorbidities and management in schizophrenia. Methods: This study employed retrospective, multi-center, observational design to investigate the demographic & clinical profiles of patients diagnosed with schizophrenia. Data was collected from patient records across diverse healthcare settings in India. Results: The study population comprised total of 5085 individuals, with mean age of 48.5 years. The most common positive symptom reported was hallucinations (19.5%), followed by delusions (17.8%). Lack of motivation was the most frequent negative symptom (21.9%) & difficulties with working memory were most prevalent cognitive symptoms (33.7%). Catatonia was observed in (12.8%) of patients. Anxiety was reported by (10.9%) of patients, Obsessive-compulsive disorder (OCD) was present in (16.8%) of patients, & (13.6%) reported substance abuse. Depression was identified in (20.8%) of patients with (13.8%) taking antidepressants. There was significant reduction in the PANSS (Positive and Negative Syndrome Scale) score from baseline. Olanzapine was frequently prescribed antipsychotic, with escitalopram commonly used as adjunct therapy. Conclusion: The study shows a high prevalence of schizophrenia with diverse symptoms, co-morbidities, and treatment approaches. The study highlights the need for better data refinement and standardization to improve research accuracy and patient care in schizophrenia.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dr Nitin Kapure, Dr Siddharth Nikam, Dr Mayur Mayabhate, Dr Akhilesh Sharma

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet. 2016 Jul 2;388(10039):86-97. doi: 10.1016/S0140-6736(15)01121-6. Epub 2016 Jan 15. PMID: 26777917; PMCID: PMC4940219.
[2] Kooyman I, Dean K, Harvey S, Walsh E. Outcomes of public concern in schizophrenia. Br J Psychiatry Suppl 2007; 50: s29-36.
[3] Marwaha S, Johnson S. Schizophrenia and employment-a review. Soc Psychiatry Psychiatr Epidemiol 2004; 39: 337-49.
[4] Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry 2014; 13: 153-60.
[5] Joyce EM, Roiser JP. Cognitive heterogeneity in schizophrenia. Curr Open Psychiatry 2007; 20: 268-72.
[6] Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry 2001; 50: 884-97.
[7] Addington J, Heinssen R. Prediction and prevention of psychosis in youth at clinical high risk. Annu Rev Clin Psychol 2012; 8: 269-89.
[8] Lewandowski KE, Cohen BM, Ongur D. Evolution of neuropsychological dysfunction during the course of schizophrenia and bipolar disorder. Psychol Med 2011; 41: 225-41.
[9] Diagnostic and Statistical Manual of Mental Disorders. 4th ed., text revision. Washington, D.C.: American Psychiatric Association, 2000:297-343.
[10] https://www.mayoclinic.org/diseases-conditions/schizophrenia/symptoms-causes/syc 20354443
[11] Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: Classification and criteria changes. World Psychiatry. 2013 Jun;12(2):92-8. doi: 10.1002/wps.20050. PMID: 23737408; PMCID: PMC3683251
[12] Maj M, van Os J, De Hert M, Gaebel W, Galderisi S, Green MF, Guloksuz S, Harvey PD, Jones PB, Malaspina D, McGorry P, Miettunen J, Murray RM, Nuechterlein KH, Peralta V, Thornicroft G, van Winkel R, Ventura J. The clinical characterization of the patient with primary psychosis aimed at personalization of management. World Psychiatry. 2021 Feb;20(1):4-33. doi: 10.1002/wps.20809. PMID: 33432763; PMCID: PMC7801854.
[13] Egerton A, Grace AA, Stone J, Bossong MG, Sand M, McGuire P. Glutamate in schizophrenia: Neurodevelopmental perspectives and drug development. Schizophr Res. 2020 Sep;223:59-70. doi: 10.1016/j.schres.2020.09.013. Epub 2020 Oct 16. PMID: 33071070.
[14] Pasternak O, Kelly S, Sydnor VJ, Shenton ME. Advances in microstructural diffusion neuroimaging for psychiatric disorders. Neuroimage. 2018 Nov 15;182:259-282. doi: 10.1016/j.neuroimage.2018.04.051. Epub 2018 May 2. PMID: 29729390; PMCID: PMC6420686
[15] Menniti FS, Chappie TA, Schmidt CJ (2021): PDE10A inhibitors clinical failure or window into antipsychotic drug action? Front Neu rosci 14:600178.
[16] Ochoa, S., Usall, J., Cobo, J., Labad, X., & Kulkarni, J. (2012). Gender Differences in Schizophrenia and First-Episode Psychosis: A Comprehensive Literature Review. Schizophrenia Research and Treatment, 2012, 1-9. https://doi.org/10.1155/2012/916198
[17] McGrath, J., Saha, S., Chant, D., & Welham, J. (2008). Schizophrenia: A Concise Overview of Incidence, Prevalence, and Mortality. Epidemiologic Reviews, 30(1), 67-76. https://doi.org/10.1093/epirev/mxn001
[18] Favrod, J., Nguyen, A., Chaix, J., Pellet, J., Frobert, L., Fankhauser, C., Ismailaj, A., Brana, A., Tamic, G., Suter, C., Rexhaj, S., Golay, P., & Bonsack, C. (2019). Improving Pleasure and Motivation in Schizophrenia: A Randomized Controlled Clinical Trial. Psychotherapy and Psychosomatics, 88(2), 84-95. https://doi.org/10.1159/000496479
[19] Berman, I., Viegner, B., Merson, A., Allan, E., Pappas, D., & Green, A. I. (1997). Differential relationships between positive and negative symptoms and neuropsychological deficits in schizophrenia. Schizophrenia Research, 25(1), 1-10. https://doi.org/10.1016/S0920-9964(96)00098-9
[20] Cvetić T, Vuković O. Cognitive deficit in schizophrenia: comparative analysis of positive and negative subtype and predictors of positive subtype. Psychiatr Danub. 2006 Jun;18(1-2):4-11. PMID: 16804494.
[21] Kleinhaus, K., Harlap, S., Perrin, M. C., Manor, O., Weiser, M., Harkavy-Friedman, J. M., Lichtenberg, P., & Malaspina, D. (2012). Catatonic Schizophrenia: A Cohort Prospective Study. Schizophrenia Bulletin, 38(2), 331-337. https://doi.org/10.1093/schbul/sbq087
[22] Krishna, K. R., Maniar, R. C., & Harbishettar, V. S. (2011). A comparative study of “Idiopathic catatonia” with catatonia in schizophrenia. Asian Journal of Psychiatry, 4(2), 129-133. https://doi.org/10.1016/j.ajp.2011.04.007
[23] Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009 Mar;35(2):383-402. doi: 10.1093/schbul/sbn135. Epub 2008 Nov 14. PMID: 19011234; PMCID: PMC2659306.
[24] Etchecopar-Etchart, D., Korchia, T., Loundou, A., Llorca, P.-M., Auquier, P., Lançon, C., Boyer, L., & Fond, G. (2021). Comorbid Major Depressive Disorder in Schizophrenia: A Systematic Review and Meta-Analysis. Schizophrenia Bulletin, 47(2), 298-308. https://doi.org/10.1093/schbul/sbaa153
[25] Molloy, C., Conroy, R. M., Cotter, D. R., & Cannon, M. (2011). Is Traumatic Brain Injury A Risk Factor for Schizophrenia? A Meta-Analysis of Case-Controlled Population-Based Studies. Schizophrenia Bulletin, 37(6), 1104-1110. https://doi.org/10.1093/schbul/sbr091
[26] Chu, R. S. T., Chong, R. C. H., Chang, D. H. H., Shan Leung, A. L., Chan, J. K. N., Wong, C. S. M., & Chang, W. C. (2024). The risk of stroke and post-stroke mortality in people with schizophrenia: A systematic review and meta-analysis study. Psychiatry Research, 332, 115713. https://doi.org/10.1016/j.psychres.2024.115713