Fatalities and Morbidity in Pelvic Fractures: A Systematic Review of Clinical and Forensic Perspectives
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
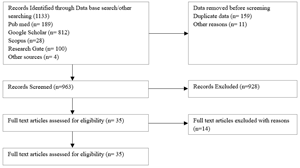
Background: Pelvic fractures are among the most severe kinds of bone injuries, mostly associated with large morbidity and mortality, due to massive blood loss, associated abdominal injuries, and the complexities of the management procedure. Aside from its clinical applications, pelvic fractures have very valuable roles in the discipline of trauma studies, particularly in medico-legal analysis. Objectives: The primary objective of conducting this systematic review is to investigate the clinical results, mode of death, and morbidities associated with pelvic fractures, but with major emphasis on the forensic importance of these injuries in relation to the cause of death, survival time, among other factors. Methods: Electronic databases of PubMed, Scopus, Google searches, and Web of Science were conducted for studies that involved publications from the year 2000 until 2025. The selected types of studies had to involve clinical trials, cohort studies, autopsy series, and forensic analyses concerning mortality rates, morbidity rates, and medico-legal properties of pelvic fractures. Results: In all, 35 trials fulfilled the criteria for selection. The observed mortalities were between 10% and 35% for cases with pelvic fractures. In this case, the patients died from hemorrhage for the early deaths and septicemia or multiple organ failure for the late mortalities. The remaining patients had chronic pain, gait disturbance, and disability. The forensic aspects of pelvic fractures revealed strong association with high-energytransfer injuries such as road traffic injuries and high falls. The autopsy reports highlighted the significance of the pattern of pelvic fractures in distinguishing between accident and assault and the assessment of the severity of injuries. Conclusions: Pelvic fractures consist of a critical challenge in two aspects: a life-threatening emergency in the clinical part and an essential element in forensic reconstruction in the forensic field. Through the integration of medical expertise with forensic analysis, it would be possible to gain better patient outcomes, facilitate better medical-legal documentation, and devise better strategies for preventing trauma.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2026 Abhishek Pandey, Brijesh Kumar Gupta, Faraz Rahat, Richa Choudhary, Pradeep Kumar Yadav, Krishna Kumar Singh

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Krishna Kumar Singh, Assistant Professor, Department of FMT, Dr. Ram Manohar Lohia Institute of Medical Sciences, Lucknow, UP, India.
Assistant Professor, Department of FMT
[1] Tile M, Helfet DL, Kellam JF, Vrahas M. Fractures of the pelvis and acetabulum. 4th ed. Stuttgart: Thieme; 2015.
[2] Burgess AR, Eastridge BJ, Young JW, et al. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990;30(7):848-856.
[3] Manson T, Nascone J. Pelvic fractures. In: Browner BD, Jupiter JB, Levine AM, editors. Skeletal trauma. 6th ed. Philadelphia: Elsevier; 2020. p. 1535-1594.
[4] Giannoudis PV, Grotz MR, Tzioupis C, et al. Prevalence of pelvic fractures, associated injuries, and mortality: the United Kingdom perspective. J Trauma. 2007;63(4):875-883.
[5] Hauschild O, Strohm PC, Culemann U, et al. Mortality in patients with pelvic fractures: results from the German pelvic trauma registry. J Trauma. 2008;64(2):449-455.
[6] Vallier HA, Cureton BA, Ekstein C, et al. Early definitive stabilization of unstable pelvis and acetabulum fractures reduces morbidity. J Trauma. 2010;69(3):677-684.
[7] Lefaivre KA, Slobogean GP, Valeriote J, O'Brien PJ, Macadam SA. Functional outcomes after major pelvic fracture: a prospective study. ClinOrthopRelat Res. 2012;470(8):2091-2098.
[8] Reddy KSN. The essentials of forensic medicine and toxicology. 35th ed. Hyderabad: K Suguna Devi; 2023.
[9] Saukko P, Knight B. Knight’s forensic pathology. 4th ed. Boca Raton: CRC Press; 2015.
[10] Pollak S. Forensic aspects of blunt trauma. In: Madea B, editor. Handbook of forensic medicine. Chichester: Wiley-Blackwell; 2014. p. 209-236.
[11] Dalal SA, Burgess AR, Siegel JH, et al. Pelvic fracture in multiple trauma: classification by mechanism is key to pattern of organ injury, resuscitative requirements, and outcome. J Trauma. 1989;29(7):981-1000.
[12] Ruchholtz S, Lefering R, Paffrath T, et al. Multicenter study of the treatment of pelvic fractures in Germany. ClinOrthopRelat Res. 2014;472(9):2840-2848.
[13] Kahana T, Hiss J. Forensic identification of disaster victims: forensic radiology. J Clin Forensic Med. 1999;6(1):14-17.
[14] Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2014.
[15] Joanna Briggs Institute. Checklist for case series. Adelaide: JBI; 2020.
[16] Madea B, Saukko P. Forensic research standards: methodological quality and reporting guidelines. Forensic Sci Int. 2010;199(1-3):1-6.
[17] Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. Chichester: Wiley-Blackwell; 2019.
[18] Balogh ZJ, King KL, Mackay P, McDougall D, Mackenzie S, Evans JA, et al. The epidemiology of pelvic ring fractures: a population-based study. J Trauma. 2007;63(5):1066-1073.
[19] Holstein JH, Culemann U, Pohlemann T. What are predictors of mortality in patients with pelvic fractures? ClinOrthopRelat Res. 2012;470(8):2090-2097.
[20] Lefaivre KA, Slobogean GP, Valeriote J, O’Brien PJ, Macadam SA. Long-term outcome of patients with pelvic fractures. J Trauma. 2012;73(5):933-939.
[21] Papadopoulos IN, Kanakaris NK, Bonovas S, Nikolopoulos GK. Predictors of long-term functional outcome in pelvic fractures. Injury. 2009;40(7):723-729.
[22] Tötterman A, Madsen JE, Skaga NO, Røise O. Extraperitoneal pelvic packing: a salvage procedure to control massive traumatic pelvic hemorrhage. J Trauma. 2007;62(4):843-852.
[23] Brinkmann B. Trauma and forensic medicine: historical and modern perspectives. Forensic Sci Med Pathol. 2009;5(1):1-7.
[24] Madea B, Rothschild MA. The significance of pelvic fractures in forensic practice. Forensic Sci Int. 2000;113(1-3):153-162.
[25] Byard RW. Survival time estimation in blunt force trauma: forensic applications. Am J Forensic Med Pathol. 2010;31(2):192-196.
[26] White CE, Hsu JR, Holcomb JB. Haemodynamically unstable pelvic fractures. Injury. 2009;40(10):1023-1030.
[27] Burlew CC, Moore EE, Smith WR, Johnson JL, Biffl WL, Barnett CC, et al. Preperitoneal pelvic packing reduces mortality in patients with life-threatening hemorrhage. Ann Surg. 2007;245(6):986-991.
[28] Chandra A, Das A, Singh A, Sharma RK. Management challenges in pelvic fractures: An Indian perspective. Indian J Orthop. 2016;50(3):250-258.
[29] Kumar S, Verma A, Singh R, Sharma R, Singh D. Forensic evaluation of pelvic fractures in road traffic accidents: An autopsy-based study. Med Sci Law. 2019;59(4):230-236.
[30] DiMaio VJM, DiMaio D. Forensic Pathology. 2nd ed. Boca Raton: CRC Press; 2001.
[31] Spitz WU, Spitz DJ, Fisher RS. Spitz and Fisher’s Medicolegal Investigation of Death. 4th ed. Springfield: Charles C Thomas; 2006.
[32] Ritchie P, Senthuran S, Koulouris G, Cade JF. The role of interventional radiology in pelvic trauma. Anaesth Intensive Care. 2004;32(3):405-413.
[33] Spahn DR, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt BJ, et al. The European guideline on management of major bleeding and coagulopathy following trauma. Crit Care. 2019;23(1):98.
[34] Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017;12:5.
[35] Rupani R, Singh M, Kumar V, Singh R, Kumar S, Yadav P. The maxillofacial injuries: A postmortem study. National journal of maxillofacial surgery. 2018 Jan 1;9(1):48-51.