Clinical Profile, Severity Assessment, Management and Outcomes of Acute Organophosphate Poisoning: A Prospective Observational Study
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
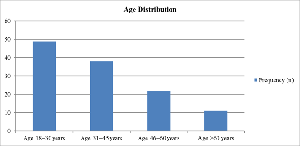
Objectives: To study the epidemiological profile, clinical presentation, severity assessment using the Peradeniya Organophosphorus Poisoning (POP) score, treatment patterns, and clinical outcomes of patients with acute organophosphate poisoning. Methods: This prospective observational study was conducted in the Emergency Medicine Department of a tertiary care hospital in Western India from September 2023 to September 2025. A total of 120 patients with confirmed acute organophosphate poisoning were included. Demographic details, clinical features, POP score at admission, atropine requirement, ICU admission, need for mechanical ventilation, and in-hospital outcomes were recorded. Statistical analysis was performed using the Chi-square test, and a p-value < 0.05 was considered statistically significant. Results: The mean age of patients was 33.85 ± 14.65 years, with a marked male predominance (87.5%). Most patients were from rural areas and suicidal ingestion was the commonest mode of poisoning. Based on POP score at admission, 38.3% of patients had mild, 59.2% had moderate, and 2.5% had severe poisoning. ICU admission and mechanical ventilation were required in 22.5% of patients each. Mean atropine requirement increased with severity of poisoning (29.04 mg in mild, 55.44 mg in moderate, and 143.33 mg in severe cases). Overall mortality was 10% and increased significantly with POP score severity (χ² = 13.42, p = 0.0006). Conclusion: Acute organophosphate poisoning predominantly affects young adults and continues to cause significant morbidity and mortality. The POP score is a simple and effective bedside tool for early severity assessment and outcome prediction. Higher POP scores are associated with increased atropine requirement, need for intensive care, mechanical ventilation, and mortality. Routine use of POP scoring in emergency departments can aid in early triage, appropriate management, and optimal resource utilization.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2026 Jigarkumar B. Gosai, MD, Ramchandani Himanshu D, MD, Vidur V Joshi, MD

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Ramchandani Himanshu D, MD, Senior Resident, Department of Emergency Medicine, Government Medical College, Vadodara, Gujarat, India. Past Affiliation: 3rd Year Resident, Department of Emergency Medicine, B. J. Medical College, Civil Hospital, Asarwa, Ahmedabad, Gujarat, India.
Senior Resident, Department of Emergency Medicine, Government Medical College, Vadodara, Gujarat, India.
Past Affiliation: 3rd Year Resident, Department of Emergency Medicine, B. J. Medical College, Civil Hospital, Asarwa, Ahmedabad, Gujarat, India.
[1] Senanayake N, Karalliedde L. A scoring system to predict prognosis in organophosphate poisoning. Hum Exp Toxicol. 1993;12(4):297–299.
[2] Davies JOJ, Eddleston M, Buckley NA. Predicting outcome in acute organophosphate poisoning. Clin Toxicol. 2008;46(5):459–465.
[3] Eddleston M, Buckley NA, Eyer P, Dawson AH. Management of acute organophosphorus pesticide poisoning. Lancet. 2008;371(9612):597–607.
[4] Gunnell D, Eddleston M. Suicide by intentional ingestion of pesticides. Int J Epidemiol. 2003;32(6):902–909.
[5] Chugh SN, Dushyant, Ram S, Arora B. Incidence and outcome of organophosphate poisoning in northern India. J Assoc Physicians India. 1998;46(6):572–575.
[6] Banday TH, Tathineni B, Desai MS, Naik V. Predictors of morbidity and mortality in organophosphorus poisoning. Indian J Crit Care Med. 2015;19(6):312–316.
[7] Muley A, Shah C, Lakhani J. Organophosphate poisoning: Correlation of POP score with severity and outcome. J Assoc Physicians India. 2014;62(2):45–47.
[8] Agarwal SB. A clinical, biochemical, neurobehavioral study of organophosphorus poisoning. Environ Res. 1993;62(1):63–70.
[9] Yamashita M, Tanaka J, Ando Y. Human mortality in organophosphate poisoning. Vet Hum Toxicol. 1997;39(2):84–85.
[10] Karalliedde L, Senanayake N. Organophosphorus insecticide poisoning. Br J Anaesth. 1989;63(6):736–750.
[11] Senanayake N, Karalliedde L. A simple clinical score to predict outcome in organophosphorus poisoning. Br J Anaesth. 1987;59:137–142.
[12] Kamath SD, Radhika K, Pai M, et al. Clinical profile and outcome of organophosphorus poisoning. J Clin Diagn Res. 2016;10:OC01–OC04.
[13] Patil A, Peshattiwar V, Kothari R. Clinical profile and outcome of organophosphate poisoning. Int J Adv Med. 2017;4:134–139.
[14] Sinha R, Singh S, Yadav S. Clinical profile and outcome of organophosphate poisoning. J Assoc Physicians India. 2014;62:29–32.
[15] Murali R, Bhalla A, Singh D, et al. Organophosphate poisoning: predictors of mortality. Indian J Crit Care Med. 2012;16:146–150.
[16] Banerjee I, Tripathi SK, Roy AS. Clinico-epidemiological profile of organophosphate poisoning. J Indian Med Assoc. 2012;110:89–92.
[17] Malaviya AN, Jindal AK, et al. Correlation of POP score with outcome in organophosphate poisoning. Indian J Anaesth. 2015;59:68–73.
[18] Buckley NA, Eddleston M, Li Y, et al. Oximes for acute organophosphate poisoning. Cochrane Database Syst Rev. 2011;2:CD005085.
[19] Peter JV, Sudarsan TI, Moran JL. Clinical features of organophosphate poisoning. Crit Care. 2014;18:245.
[20] World Health Organization. Preventing suicide: a global imperative. WHO; 2014