The Impact of a TPA Unit during the COVID-19 Pandemic on Inpatient Length of Stay and Outcomes for Ischemic Stroke
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
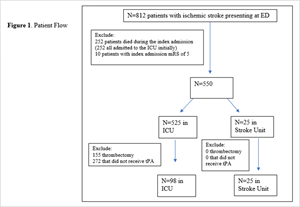
Background: Resource allocation can be problematic in ischemic stroke receiving IV thrombolysis (tPA) during COVID-19 pandemic as only a subset requires critical care interventions. It is also unknown whether the usage of non-ICU stroke unit for post-tPA care has better patient outcome compared to ICU. Methods: A pilot study in a single tertiary medical center, in which one-bed tPA unit was created in a non-ICU Stroke Unit during the COVID-19 pandemic, with the provision of ICU level of nursing care. We included 123 consecutive ischemic stroke patients treated with tPA, included in an institutional registry between October 2020 and December 2021. The primary outcome of interest was inpatient length of stay (LOS). The secondary outcome of interest was the 90-day clinical outcomes. Results: Amongst a total of 123 patients, control group consisted of 98 (79.7%) patients who received standard post-tPA care in an ICU, and the study group consisted of 25 (20.3%) patients who received standard post-tPA care in Stroke Unit. There were no statistically significant differences between the 2 groups in terms of median LOS or median 90-day NIHSS. However, the median 90-day mRS was lower in the study group compared to the ICU group (0 IQR (0-1) vs. 2 (1-5); P=0.0011). The 90-day death outcome was also lower in the study group compared to the control (0% vs. 25.5%, P<0.05). Conclusion: Providing post-tPA care in non-ICU with the ICU level of neurological nursing care did not reduce length of stay but improved the functional outcome for post-tPA ischemic stroke.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2024 Akanksha Gulati, MBBS, Eliza Grigoriciuc, MD, Shravan Sivakumar, MBBS, Brian Silver, MD, Nils Henninger, MD, PhD, Dr. Med, Rakhee Lalla, DO, Majaz Moonis, MD, Adalia H. Jun-O’Connell, MD, MBA

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Faigle, R., et al., Predictors of critical care needs after IV thrombolysis for acute ischemic stroke. PLoS One, 2014. 9(2): p. e88652.
Chang, A., et al., Shorter Intensive Care Unit Stays? The Majority of Post-Intravenous tPA (Tissue-Type Plasminogen Activator) Symptomatic Hemorrhages Occur Within 12 Hours of Treatment. Stroke, 2018. 49(6): p. 1521-1524.
Sadaka, F., et al., Do All Acute Stroke Patients Receiving tPA Require ICU Admission? J Clin Med Res, 2018. 10(3): p. 174-177.
Hick, J.L., et al., Crisis Standards of Care and COVID-19: What Did We Learn? How Do We Ensure Equity? What Should We Do? NAM Perspect, 2021. 2021.
Langhorne, P. and S. Ramachandra, Organised inpatient (stroke unit) care for stroke: network meta-analysis. Cochrane Database Syst Rev, 2020. 4(4): p. Cd000197.
Faigle, R., et al., Low-Intensity Monitoring After Stroke Thrombolysis During the COVID-19 Pandemic. Neurocrit Care, 2020. 33(2): p. 333-337.
Faigle, R., et al., Safety Trial of Low-Intensity Monitoring After Thrombolysis: Optimal Post Tpa-Iv Monitoring in Ischemic STroke (OPTIMIST). Neurohospitalist, 2020. 10(1): p. 11-15.
Alexandrov, A.W., et al., Direct stroke unit admission of intravenous tissue plasminogen activator: safety, clinical outcome, and hospital cost savings. Ther Adv Neurol Disord, 2016. 9(4): p. 304-9.
Powers, W.J., et al., Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke, 2019. 50(12): p. e344-e418.
http://www.strobe-statement.org.
Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev, 2013. 2013(9): p. Cd000197.
Khan, S., A. Soto, and E.B. Marsh, Resource Allocation: Stable Patients Remain Stable 12-24 h Post-tPA. Neurocrit Care, 2020. 33(2): p. 582-586.
Williams, L.S., E.Y. Yilmaz, and A.M. Lopez-Yunez, Retrospective assessment of initial stroke severity with the NIH Stroke Scale. Stroke, 2000. 31(4): p. 858-62.
Jeon, C.Y., et al., On the role of length of stay in healthcare-associated bloodstream infection. Infect Control Hosp Epidemiol, 2012. 33(12): p. 1213-8.
Dziegielewski, C., et al., Delirium and Associated Length of Stay and Costs in Critically Ill Patients. Crit Care Res Pract, 2021. 2021: p. 6612187.
Stewart, S., et al., Impact of healthcare-associated infection on length of stay. J Hosp Infect, 2021. 114: p. 23-31.
Zang, K., et al., The effect of early mobilization in critically ill patients: A meta-analysis. Nurs Crit Care, 2020. 25(6): p. 360-367.
Jørgensen, H.S., et al., The effect of a stroke unit: reductions in mortality, discharge rate to nursing home, length of hospital stay, and cost. A community-based study. Stroke, 1995. 26(7): p. 1178-82.
Ganesh, A., et al., Integrated systems of stroke care and reduction in 30-day mortality: A retrospective analysis. Neurology, 2016. 86(10): p. 898-904.