From Blues to Breakdown: A Psychiatric Reappraisal of Postpartum Psychosis with Real-World Cases
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
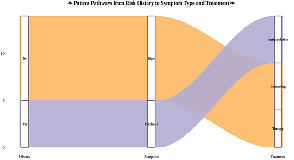
Background: Postpartum psychiatric illnesses, from the ubiquitous but generally self-limited baby blues to the comparatively unusual but potentially fatal postpartum psychosis, remain under-recognized in maternal mental illness. Despite growing attention, underdiagnosis, stigma, and absence of standardized diagnostic classification remain a threat to early detection and treatment. Aim and Objective: The purpose of this research is to critically assess current literature on the etiology, risk factors, prevention, and treatment of postpartum psychiatric disorders, with two model clinical vignettes. The aim is to discuss the multifaceted etiology, pathways, and management of these disorders, and to ask: Why is postpartum psychosis yet to be officially recognized considering its disastrous outcomes? Methods: The narrative review with systematic elements consisted of 10 peer-reviewed papers of different geographical and methodological backgrounds. Two clinical cases from practice were included to provide context and enhance the scope of the evidence. Inclusion criteria were papers on postpartum blues, depression, or psychosis in women up to one year postpartum. Exclusion criteria were literature that was not in English and non-clinical outcome studies. Results: Five studies were initially synthesized, followed by Case 1, a 35-year-old woman with postpartum depression. The other five studies were examined before Case 2, a 32-year-old woman with recurrent postpartum psychosis. The common risk factors were primiparity, bipolar disorder, immune dysregulation, and psychosocial stress. Lithium and antipsychotics were always indicated for postpartum psychosis, and SSRIs and psychosocial interventions were helpful for depression. Case 1 presented early-onset depressive symptoms like refusal to eat, tearfulness, and somatic complaints on Day 3 postpartum. Case 2, with a history of a previous psychotic episode following the death of her first child, presented relapse symptoms of hallucinations and disorganized thinking following the second delivery, again on Day 3 postpartum. Conclusion: Postpartum psychiatric disorders are multifactorial, recurrent, and underdiagnosed. There is an urgent need for early screening, Diagnostic and Statistical Manual of Mental Disorders (DSM) reclassification of postpartum psychosis, and integrated maternal mental health services.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Nair Deepa Balasubramanian, Gayathri V., Vijunath Thilakan, Jamila Hameed

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Nair Deepa Balasubramanian, Department of Psychiatry, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, 678103, India.
Department of Psychiatry, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, 678103, India.
Gayathri V., Department of Psychiatry, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, 678103, India.
Department of Psychiatry, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, 678103, India.
Vijunath Thilakan, Department of Psychiatry, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, 678103, India.
Department of Psychiatry, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, 678103, India.
Jamila Hameed, Department of Psychiatry, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, 678103, India.
Research Mentor, Emiratus Professor, Karuna Medical College, Kerala University of Health Sciences, Kerala, India
[1] Rai S, Pathak A, Sharma I. Postpartum psychiatric disorders: Early diagnosis and management. Indian journal of psychiatry. 2015 Jul 1;57(Suppl 2):S216-21.
[2] Liu Y, Guo N, Li T, Zhuang W, Jiang H. Prevalence and associated factors of postpartum anxiety and depression symptoms among women in Shanghai, China. Journal of affective disorders. 2020 Sep 1;274:848-56.
[3] Le Donne M, Mento C, Settineri S, Antonelli A, Benvenga S. Postpartum mood disorders and thyroid autoimmunity. Frontiers in Endocrinology. 2017 May 4;8:91.
[4] Hopkins J, Marcus M, Campbell SB. Postpartum depression: a critical review. Psychol Bull. 1984 May;95(3):498-515. PMID: 6399755.
[5] Garapati J, Jajoo S, Aradhya D, Reddy LS, Dahiphale SM, Patel DJ, Jyotsna G, Deeksha HS, srivani Reddy L, Dahiphale SM. Postpartum mood disorders: insights into diagnosis, prevention, and treatment. Cureus. 2023 Jul 19;15(7).
[6] Brockington I. Postpartum psychiatric disorders. Lancet. 2004 Jan 24;363(9405):303-10. doi: 10.1016/S0140-6736(03)15390-1. PMID: 14751705.
[7] Keshavarzi F, Yazdchi K, Rahimi M, Rezaei M, Farnia V, Davarinejad O, Abdoli N, Jalili M. Post partum depression and thyroid function. Iran J Psychiatry. 2011 Summer;6(3):117-20. PMID: 22952534; PMCID: PMC3395948.
[8] Ghaedrahmati M, Kazemi A, Kheirabadi G, Ebrahimi A, Bahrami M. Postpartum depression risk factors: A narrative review. J Educ Health Promot. 2017 Aug 9;6:60. doi: 10.4103/jehp.jehp_9_16. PMID: 28852652; PMCID: PMC5561681.
[9] Rahmanian H. Post Natal Depression in Iran. European Psychiatry. 2015 Mar;30(S1):1-.
[10] Hazelgrove K. The role of the immune system in postpartum psychosis. Brain Behav Immun Health. 2021 Sep 29;18:100359. doi: 10.1016/j.bbih.2021.100359. PMID: 34704078; PMCID: PMC8521124.
[11] Osborne LM. Recognizing and Managing Postpartum Psychosis: A Clinical Guide for Obstetric Providers. Obstet Gynecol Clin North Am. 2018 Sep;45(3):455-468. doi: 10.1016/j.ogc.2018.04.005. PMID: 30092921; PMCID: PMC6174883.
[12] Dye C, Lenz KM, Leuner B. Immune system alterations and postpartum mental illness: evidence from basic and clinical research. Frontiers in global women's health. 2022 Feb 10;2:758748.
[13] Nguyen K, Mukona LT, Nalbandyan L, Yar N, St Fleur G, Mukona L, Hernandez E, Lamberty N. Peripartum Complications as Risk Factors for Postpartum Psychosis: A Systemic Review. Cureus. 2022 Sep 16;14(9):e29224. doi: 10.7759/cureus.29224. PMID: 36159350; PMCID: PMC9495292.
[14] Brummelte S, Galea LA. Postpartum depression: Etiology, treatment and consequences for maternal care. Hormones and behavior. 2016 Jan 1;77:153-66.
[15] Meltzer-Brody S, Howard LM, Bergink V, Vigod SN, Jones I, Munk-Olsen T, Honikman S, Milgrom J. Postpartum psychiatric disorders. Nat Rev Dis Primers. 2018 Apr 26.
[16] Jain S, Singhai K, Pareek V, Nebhinani N. Comprehensive antenatal to postpartum care of patient with bipolar disorder: a case report. Case Reports in Perinatal Medicine. 2019 Sep 25;8(2):20180057.
[17] Jairaj C, Seneviratne G, Bergink V, Sommer IE, Dazzan P. Postpartum psychosis: A proposed treatment algorithm. J Psychopharmacol. 2023 Oct;37(10):960-970. doi: 10.1177/02698811231181573. Epub 2023 Jul 29. PMID: 37515460; PMCID: PMC10612381.
[18] Lawson A, Dalfen A. Examination of a four-step treatment algorithm for postpartum psychosis. BMJ Ment Health. 2016 Feb 1;19(1):25-.
[19] Spinelli M. Postpartum psychosis: a diagnosis for the DSMV. Arch Womens Ment Health. 2021 Oct;24(5):817-822. doi: 10.1007/s00737-021-01175-8. Epub 2021 Sep 8. PMID: 34494144.
[20] Bergink V, Rasgon N, Wisner KL. Postpartum Psychosis: Madness, Mania, and Melancholia in Motherhood. Am J Psychiatry. 2016 Dec 1;173(12):1179-1188. doi: 10.1176/appi.ajp.2016.16040454. Epub 2016 Sep 9. PMID: 27609245.
[21] Rommel AS, Molenaar NM, Gilden J, Kushner SA, Westerbeek NJ, Kamperman AM, Bergink V. Long-term outcome of postpartum psychosis: a prospective clinical cohort study in 106 women. International journal of bipolar disorders. 2021 Dec;9:1-0.
[22] Davies W. Understanding the pathophysiology of postpartum psychosis: Challenges and new approaches. World journal of psychiatry. 2017 Jun 22;7(2):77.