##plugins.themes.bootstrap3.article.main##
Abstract
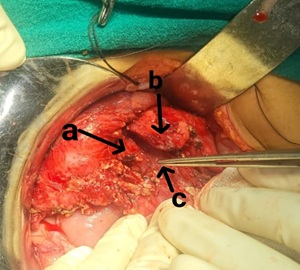
Background: Pancreatic trauma is a rare but challenging condition due to its retroperitoneal location and nonspecific clinical presentation. This study evaluates the outcomes of pancreatic trauma patients in a tertiary care center. Methods: A prospective study was conducted on patients diagnosed with pancreatic trauma between January 2019 and April 2025. Data on demographics, injury grading, management strategies, complications, and outcomes were analyzed. Results: Out of 18 patients with pancreatic trauma, 8 were managed conservatively, while 10 underwent surgical intervention. Morbidity was significantly higher in Grade III and above injuries (p<0.05). Mortality was observed in 2 cases, predominantly with associated injuries and delayed diagnosis. Conclusion: Early recognition and appropriate grading of pancreatic trauma significantly influence outcomes. Surgical intervention is often reserved for higher-grade injuries or those with complications such as ductal disruption or associated organ injury.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Javid Iqbal, Ab Hamid Wani, Bisma Latif, Gurbir Singh, Satish Parihar

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Jurkovich GJ, Carrico CJ. Pancreatic trauma. Surg Clin North Am. 1990 Jun;70(3):575-93.
[2] Phelan HA, Velmahos GC, Jurkovich GJ. Management of pancreatic trauma. Am Surg. 2009 Jul;75(7):628-35.
[3] Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Champion HR, Hirshberg A. Organ injury scaling: Spleen and liver (1994 revision). J Trauma. 1995 Mar;38(3):323-4.
[4] Akhrass R, Yaffe MB, Brandt CP, Reigle M, Fallon WF, Malangoni MA. Pancreatic trauma: a ten-year multi-institutional experience. Am Surg. 1997 Jul;63(7):598-604.
[5] Bradley EL 3rd. Operative management of pancreatic trauma. Am J Surg. 1985 Dec;150(6):726-8.
[6] Gupta A, Stuhlfaut JW, Fleming KW, Lucey BC, Soto JA. Blunt trauma of the pancreas and biliary tract: A multimodality imaging approach to diagnosis. Radiographics. 2004 Sep-Oct;24(5):1381-95.
[7] Patton JH Jr, Lyden SP, Croce MA, Pritchard FE, Minard G, Kudsk KA, et al. Pancreatic trauma: A simplified management guideline. J Trauma. 1997 Mar;42(3):582-6.
[8] Krige JE, Nicol AJ, Navsaria PH. Emergency pancreatectomy for complex pancreatic trauma. Arch Surg. 2009 Aug;144(8):745-51.
[9] Heitsch RC, Knutson CO, Fulton RL, Jones CE. Delineation of critical factors in the treatment of pancreatic trauma. Surgery. 1976 Dec;80(6):523-9.
[10] Soreide K, Weiser TG, Parks RW. Clinical update on management of pancreatic trauma. HPB 2018, 20:1099-1108.
[11] Degiannis E, Boffard K, Du Toit DF, Van Der Merwe R. Pancreatic trauma: A management guideline based on a review of 147 consecutive patients. Injury. 1996 Oct;27(8):543-7.
[12] Kaman L, Iqbal J, Pall M, Bhukal I, Behera A, Singh G, et al. Current management of pancreatic trauma. Tropical Gastrenterology. 2012 Jun;33(2): 200-6.
[13] Sharpe JP, Magnotti LJ, Weinberg JA, Zarzaur BL, Stickley SM, Scott SE, et al. Impact of a defined management algorithm on outcome after trauamatic pancreatic injury. J Trauma Acute Care Surg. 2012,72: 100-5.
[14] Menahem B, Lim C, Lahat E, Salloum C, Osseis M, Lacaze L, et al. Conservative and surgical management of pancreatic trauma in adult patients. Hepatobiliary Surg Nutr. 2016;5(6): 470-7.