Orthopaedic Surgery Interventions in Ekiti, Southwestern Nigeria: An Analysis of Patient Sociodemographics and Comorbidities
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
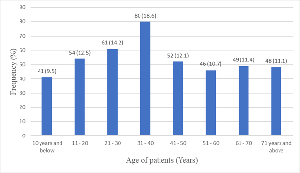
Background: Orthopaedic surgical procedures account for a substantial part of the global surgical burden. This study evaluates the demographics, indications, types, and comorbidities in patients who underwent orthopaedic interventions at Ekiti State University Teaching Hospital, Ado-Ekiti, between January 2019 and December 2024. Materials and Methods: A retrospective observational study was conducted using data collected from the theatre registers and case notes at Ekiti State University Teaching Hospital, Ado Ekiti. A total of 450 entries were reviewed, with analyses focusing on 431 complete entries. Sociodemographic information, intervention data, and comorbidities were collected and categorized accordingly. Descriptive and inferential statistics were employed for the analysis. Results: Mean age of patients was 40.7 (22.6) years. Male patients constituted 59.2% of the cohort. The most common age group for surgery was 31-40 years (18.6%). The vast majority of interventions performed were elective (86.8%), with lower limb fractures being the leading indication (46.2%). Surgical procedures were predominantly open reduction and internal fixation (38.1%). No significant association between sex and type of surgery. Statistically significant differences in mean ages across comorbidities (p < 0.001). Higher likelihood of elective surgery among patients from lower socioeconomic statuses (p < 0.05). Conclusion: This study highlights critical trends in demographic and clinical characteristics among patients undergoing orthopaedic interventions. Significant association between comorbidities, socioeconomic status, and orthopaedic surgery interventions.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2026 Dr. Moruf B, Yusuf; Dr. David B. Idowu; Dr. Oluwamuyiwa A. Dada, Dr. Emamizo U. Ojo-Maliki, Dr. Olorunwa O. Kolawole, Dr. Owolabi D. Ojo, Dr. Waheed A. Adegbiji

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Aaron FE, Ijah RFOA, Obene T. Pattern of orthopaedic case presentations at the rivers state university teaching hospital: a ten-year review. International Surgery Journal 2022; 9: 781–789.
[2] Safiri S, Kolahi A-A, Cross M, Hill C, Smith E, Carson-Chahhoud K et al. Prevalence, deaths, and disability-adjusted life years due to musculoskeletal disorders for 195 countries and territories 1990–2017. Arthritis & rheumatology 2021; 73: 702–714.
[3] Gelaw AY, Gabbe BJ, Braaf SC, McPhail S, Ekegren CL. Chronic physical health conditions and associated factors among people with serious orthopaedic injuries: A systematic review. Trauma 2021; 23: 90–100.
[4] Jin Y, Guo C, Abbasian M, Abbasifard M, Abbott JH, Abdullahi A et al. Global pattern, trend, and cross-country inequality of early musculoskeletal disorders from 1990 to 2019, with projection from 2020 to 2050. Med 2024; 5: 943–962.
[5] Aboderin I, Nanyonjo A. Musculoskeletal health conditions among older populations in urban slums in sub-Saharan Africa. Best Practice & Research Clinical Rheumatology 2017; 31: 115–128.
[6] Anderson DD, Chubinskaya S, Guilak F, Martin JA, Oegema TR, Olson SA et al. Post‐traumatic osteoarthritis: Improved understanding and opportunities for early intervention. Journal Orthopaedic Research 2011; 29: 802–809.
[7] Jiménez G, Cobo-Molinos J, Antich C, López-Ruiz E. Osteoarthritis: Trauma vs Disease. In: Oliveira JM, Pina S, Reis RL, San Roman J (eds). Osteochondral Tissue Engineering. Springer International Publishing: Cham, 2018, pp 63–83.
[8] Walani SR, Penny N, Nakku D. The global challenges of surgical congenital anomalies: evidence, models, and lessons. In: Seminars in Pediatric Surgery. Elsevier, 2023, p 151348.
[9] Ibeanusi SE, Chioma J. Pattern and outcome of femoral fractures treated in a Regional Trauma Centre in South South, Nigeria. Int Arch Orthop Surg 2019; 2: 1–9.
[10] Ugezu AI, Nze IN, Ihegihu CC, Chukwuka NC, Ndukwu CU, Ofiaeli RO. Management of femoral shaft fractures in a Tertiary Centre, South East Nigeria. Afrimedic Journal 2018; 6: 27–34.
[11] Onuoha K, Aofolajuwonlo T, Bolarinwa A, Omotayo SF. Clinical Outcomes Following Total Knee Replacement. EAS J Orthop Physiother 2022; 4: 16–19.
[12] Kremers HM, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA et al. Prevalence of total hip and knee replacement in the United States. JBJS 2015; 97: 1386–1397.
[13] Dowsey MM, Nikpour M, Choong PF. Outcomes following large joint arthroplasty: does socio-economic status matter? BMC Musculoskelet Disord 2014; 15: 148.
[14] Liu S, Qiang L, Yang Q, Fan L, Wang J, Yang Y et al. Delayed surgery is associated with adverse outcomes in patients with hip fracture undergoing hip arthroplasty. BMC Musculoskelet Disord 2023; 24: 286.
[15] Ibrahim MS, Khan MA, Nizam I, Haddad FS. Peri-operative interventions producing better functional outcomes and enhanced recovery following total hip and knee arthroplasty: an evidence-based review. BMC Med 2013; 11: 37.
[16] Alotaibi NSM, Al-Thawbani MAY, Albalawi IMR, Altalyan AAN, Alotaibi TO, Al-Asiri MAM. Patient Education: Preparing For and Recovering from Orthopedic Surgery. Tec Empresarial 2024; 6: 1016–1033.
[17] Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006; 37: 691–697.
[18] Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bulletin of the world health organization 2003; 81: 646–656.
[19] Mock C, Cherian MN. The Global Burden of Musculoskeletal Injuries: Challenges and Solutions. Clinical Orthopaedics & Related Research 2008; 466: 2306–2316.
[20] Waters R, Dey M, Laubscher R, Maqungo S, McCollum G, Nortje M et al. Drastic reduction of orthopaedic services at an urban tertiary hospital in South Africa during COVID-19: Lessons for the future response to the pandemic. South African Medical Journal 2021; 111: 240–244.
[21] Caesar U, Karlsson J, Hansson E. Incidence and root causes of delays in emergency orthopaedic procedures: a single-centre experience of 36,017 consecutive cases over seven years. Patient Saf Surg 2018; 12: 2.
[22] Ekegren CL, Beck B, Climie RE, Owen N, Dunstan DW, Gabbe BJ. Physical activity and sedentary behavior subsequent to serious orthopedic injury: A systematic review. Archives of physical medicine and rehabilitation 2018; 99: 164–177.
[23] Schatzker J. Principles of Internal Fixation. In: The Rationale of Operative Fracture Care. Springer-Verlag: Berlin/Heidelberg, 2005, pp 3–31.
[24] Scott H, Marti J, Witte P. Fracture fixation methods: principles and techniques. In: Feline Orthopaedics. CRC Press, 2022, pp 61–87.
[25] Søreide K. Epidemiology of major trauma. Journal of British Surgery 2009; 96: 697–698.
[26] Haagsma JA, Graetz N, Bolliger I, Naghavi M, Higashi H, Mullany EC et al. The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Injury prevention 2016; 22: 3–18.
[27] Stephens T, Mezei A, O’Hara NN, Potter J, Mugarura R, Blachut PA et al. When Surgical Resources are Severely Constrained, Who Receives Care? Determinants of Access to Orthopaedic Trauma Surgery in Uganda. World j surg 2017; 41: 1415–1419.
[28] Biccard BM, Madiba TE, Kluyts H-L, Munlemvo DM, Madzimbamuto FD, Basenero A et al. Perioperative patient outcomes in the African Surgical Outcomes Study: a 7-day prospective observational cohort study. The Lancet 2018; 391: 1589–1598.
[29] Martin ET, Kaye KS, Knott C, Nguyen H, Santarossa M, Evans R et al. Diabetes and risk of surgical site infection: a systematic review and meta-analysis. Infection Control & Hospital Epidemiology 2016; 37: 88–99.
[30] Panayi AC, Orkaby AR, Sakthivel D, Endo Y, Varon D, Roh D et al. Impact of frailty on outcomes in surgical patients: a systematic review and meta-analysis. The American Journal of Surgery 2019; 218: 393–400.
[31] Bernstein DN, Karhade AV, Bono CM, Schwab JH, Harris MB, Tobert DG. Sociodemographic factors are associated with Patient-Reported outcome measure completion in orthopaedic surgery: An analysis of completion rates and determinants. JBJS Open Access 2022; 7: e22.