Comparing Digital Mammography and Contrast-Enhanced Magnetic Resonance Imaging for Distinguishing Benign and Malignant Breast Lesions: A Propensity Score - Matched Retrospective Study
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
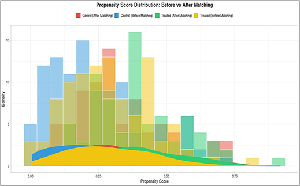
Background: Retrospective comparisons between imaging modalities commonly are confounded by systematic differences between groups between the characteristics of the patients undergoing different tests. Objective: To determine whether contrast-enhanced magnetic resonance imaging (CEMRI) discriminates malignant breast lesions better than digital mammography (DM) after the offsetting of baseline imbalances with the use of propensity score matching (PSM). Materials and Methods: Records of 480 women evaluated for suspicious breast lesions between 2020 and 2024 were reviewed retrospectively. Of these, 300 underwent DM and 180 underwent CEMRI. Propensity scores were estimated based on age, body mass index (BMI), lesion size, breast density, parity, and family history. One-to-one nearest-neighbor matching with a caliper of 0.2 standard deviations of the logit propensity score yielded 160 matched pairs. Diagnostic accuracy, confirmed by histopathology, was compared using McNemar's test. Results: Before matching, patients undergoing CEMRI were younger (mean age, 44.2 years vs 52.1 years; P < 0.001), had lower BMI (24.8 vs 26.5; P = 0.008), denser breasts (64.1% vs 38.7%; P = 0.002), lower parity (1.8 vs 2.1; P = 0.03), and higher family history prevalence (25.6% vs 14.3%; P = 0.01). After matching, covariates were balanced (all standardized mean differences < 0.1; Rubin's B = 18.3; Rubin's R = 1.1). CEMRI demonstrated higher sensitivity (94.4% vs 83.1%; P = 0.01) with comparable specificity (86.9% vs 87.5%; P = 0.73). Conclusion: After PSM correction for the patients' characteristics, CEMRI exhibited increased sensitivity in malignancy detection compared with DM in favor of deploying CEMRI in dense-breast or at-risk populations.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Shamim Hyder, Nadha Rahim, Noula Rahim, Jamila Hameed

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Shamim Hyder, Department of Radiology, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Department of Radiology, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Nadha Rahim, Department of Radiology, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Department of Radiology, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Noula Rahim, Department of Biochemistry, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Department of Biochemistry, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Jamila Hameed, Research Mentor, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Research Mentor, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
[1] Liu C, Hao X, Zhu Y, Luo C, Gao Z, Wang C, Du H, Chen L, Gao F, Huang Y, sheng Qiu B. Development and Validation of Nomograms for Preoperative Differentiation of Benign and Malignant Breast Tumors Using Ultrasound and MRI.
[2] Jung EM, Jung F, Stroszczynski C, Wiesinger I. Quantification of dynamic contrast-enhanced ultrasound (CEUS) in non-cystic breast lesions using external perfusion software. Scientific reports. 2021 Sep 3;11(1):17677.
[3] Lawson MB, Partridge SC, Hippe DS, Rahbar H, Lam DL, Lee CI, Lowry KP, Scheel JR, Parsian S, Li I, Biswas D. Comparative performance of contrast-enhanced mammography, abbreviated breast MRI, and standard breast MRI for breast cancer screening. Radiology. 2023 Aug 15;308(2):e230576.
[4] Matias MA, Sharma N, Haigh I, Millican‑Slater R, Achuthan R, Chen Y. Symposium Mammographicum 2023. Breast Cancer Research. 2023;25(2):122.
[5] Kim JH, Kessell M, Taylor D, Hill M, Burrage JW. The verification of the utility of a commercially available phantom combination for quality control in contrast-enhanced mammography. Physical and Engineering Sciences in Medicine. 2024 Dec;47(4):1491-9.
[6] Liu Y, Zhao S, Huang J, Zhang X, Qin Y, Zhong H, Yu J. Quantitative analysis of enhancement intensity and patterns on contrast-enhanced spectral mammography. Scientific Reports. 2020 Jun 17;10(1):9807.
[7] Açar ÇR, Orguc S. Comparison of performance in diagnosis and characterization of breast lesions: contrast-enhanced mammography versus breast magnetic resonance imaging. Clinical Breast Cancer. 2024 Aug 1;24(6):481-93.
[8] Yüzkan S, Cengiz D, Hekimsoy İ, Sezgin Okçu Ö, Oktay A. Diagnostic performance of contrast-enhanced mammography: comparison with MRI and mammography. Journal of Breast Imaging. 2021 Jul 1;3(4):448-54.
[9] Ghaderi KF, Phillips J, Perry H, Lotfi P, Mehta TS. Contrast-enhanced mammography: current applications and future directions. Radiographics. 2019 Nov;39(7):1907-20.
[10] Cömert D, van Gils CH, Veldhuis WB, Mann RM. Challenges and changes of the breast cancer screening paradigm. Journal of Magnetic Resonance Imaging. 2023 Mar;57(3):706-26.
[11] Elder K, Matheson J, Nickson C, Box G, Ellis J, Mou A, Shadbolt C, Park A, Tay J, Rose A, Mann GB. Contrast enhanced mammography in breast cancer surveillance. Breast Cancer Research and Treatment. 2023 Jun;199(2):221-30.
[12] Neeter LM, Raat HP, Meens-Koreman SD, van Stiphout RS, Timmermans SM, Duvivier KM, Smidt ML, Wildberger JE, Nelemans PJ, Lobbes MB. The diagnostic value of contrast-enhanced 2D mammography in everyday clinical use. Scientific Reports. 2021 Nov 15;11(1):22224.
[13] Popat P, Nandi VP, Katdare A, Haria P, Thakur M, Kulkarni S, NANDI VP, Thakur M. Diagnostic Accuracy and Incremental Value of Contrast-Enhanced Mammography Compared With Full Field Digital Mammography in a Tertiary Cancer Care Center. Cureus. 2024 Sep 4;16(9).
[14] Zhou J, Zhang Y, Miao H, Yoon GY, Wang J, Lin Y, Wang H, Liu YL, Chen JH, Pan Z, Su MY. Preoperative differentiation of HER2‐zero and HER2‐low from HER2‐positive invasive ductal breast cancers using BI‐RADS MRI features and machine learning modeling. Journal of Magnetic Resonance Imaging. 2025 Feb;61(2):928-41.