Unmet Mental Health Care Needs and Barriers to Treatment for Depression in Medical Students: A Study from North Indian State of Delhi
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
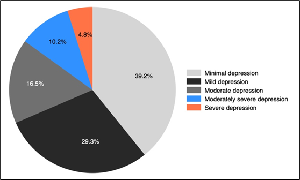
Introduction: Depression among medical students is a significant public health concern in India due to the demanding nature of medical education. The study aims to determine the prevalence of depression, evaluate unmet mental health care needs, and identify barriers to seeking help. Methodology: A cross-sectional study was conducted in 2023 among undergraduate medical students in New Delhi. The PHQ-9 assessed depression, while the BACE scale evaluated barriers to mental health care. Data analysis was performed using STATA 18. Results: Of the 413 participants, 31.4% screened positive for depression, with higher rates among second year students and those dissatisfied with academic performance or with low physical activity. Only 43.8% perceived a need for care, while 78.9% reported unmet needs. Key barriers included stigma (e.g., fear of family reactions and mental health records), attitudinal factors (e.g., preference for self-management), and instrumental challenges (e.g., academic pressures and time constraints). Conclusion: Depression is prevalent among medical students, with significant unmet care needs driven by stigma and other barriers. Interventions focusing on stigma reduction, accessibility, and mental health awareness are critical to enhancing care-seeking behavior and improving student well-being.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Aninda Debnath, Priyansha Gupta, Shweta Charag, Snigdha Basu, Nidhi Vadanere, Anita Verma

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Dutta G, Rajendran N, Kumar T, Varthya SB, Rajendran V. Prevalence of Depression Among Undergraduate Medical Students in India: A Systemic Review and Meta-Analysis. Cureus. 15(1):e33590.
[2] Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med. 2001 Sep;16(9):606-13.
[3] Clement S, Brohan E, Jeffery D, Henderson C, Hatch SL, Thornicroft G. Development and psychometric properties the Barriers to Access to Care Evaluation scale (BACE) related to people with mental ill health. BMC Psychiatry. 2012 Jun 20;12(1):36.
[4] Chaudhuri A, Mondal T, Goswami A. Prevalence of Depression, Anxiety, and Stress among Medical Students in a Developing Country during the COVID-19 Pandemic: A Pilot Study. Journal of the Scientific Society. 2020 Dec;47(3):158.
[5] Saha R, Sarkar M. Social Media Disorder Among Indian Undergraduate Medical Students and its Association with Depression: An Institution-Based Mixed-Method Study. Indian Journal of Social Psychiatry. 2020 Dec;36(4):289.
[6] Tomy C, V AL, Mathew KA, Jith A. Risk of eating disorders and its association with body image concerns, depression, anxiety and stress among medical students in a college in Kerala. Kerala Journal of Psychiatry. 2021 Sep 18;34(2):105-11.
[7] Mishra J, Panigrahi A, Samanta P, Dash K, Mahapatra P, Behera MR. Sleep quality and associated factors among undergraduate medical students during Covid-19 confinement. Clinical Epidemiology and Global Health. 2022 May 1;15:101004.
[8] Barman L, Mukhopadhyay DK, Bandyopadhyay GK. Use of Social Networking Site and Mental Disorders among Medical Students in Kolkata, West Bengal. Indian J Psychiatry. 2018;60(3):340-345.
[9] Kethawath SM, Pingali S, Kante SL, Molangur U. Mental health literacy about depression among medical students at a tertiary care hospital in South India. Telangana Journal of Psychiatry. 2020 Jun;6(1):9.
[10] Pattnaik A, Purohit S, Routray D. Original Research Article: Screening for depression and associated risk factors amongst students of a government medical college in Odisha, India. Indian Journal of Mental Health. 2020 Jul 28;7(3):202.
[11] Vala NH, Vachhani MV, Sorani AM. Study of anxiety, stress, and depression level among medical students during COVID-19 pandemic phase in Jamnagar city. National Journal of Physiology, Pharmacy and Pharmacology. 2020 Nov 30;10(12):1043-1043.
[12] Lepcha C, Kumar S, Mujeeb N, Sharma S. Anxiety and depression among medical undergraduate students and their sociodemographic correlates in Sikkim: A cross-sectional study. 2022;12(06).
[13] Wickramasinghe DP, Almeida IS, Samarasekera DN. Depression and stressful life events among medical students during undergraduate career: Findings from a medical school in South Asia. TAPS. 2019;4(1):42-7.
[14] Rana S, Taywade O, Sharma V, Hiwarkar M. Study of depression, anxiety and stress among first year Medical students in Government Medical College, Himachal Pradesh during COVID-19 pandemic. Asian Journal of Medical Sciences. 2021 Jun 1;12(6):90-4.
[15] Prabhakar V, Virk A, Saini P. Anxiety and Depression among new entrants in a Medical College. Indian Journal of Community Health. 2020 Mar 31;32(1):57-61.
[16] Martín-Rodríguez A, Gostian-Ropotin LA, Beltrán-Velasco AI, Belando-Pedreño N, Simón JA, López-Mora C, et al. Sporting Mind: The Interplay of Physical Activity and Psychological Health. Sports (Basel). 2024 Jan 22;12(1):37.
[17] Grover S, Dua D, Shouan A, Nehra R, Avasthi A. Perceived stress and barriers to seeking help from mental health professionals among trainee doctors at a tertiary care centre in North India. Asian J Psychiatr. 2019 Jan;39:143-9.
[18] White A, Shiralkar P, Hassan T, Galbraith N, Callaghan R. Barriers to mental healthcare for psychiatrists. Psychiatr bull. 2006 Oct;30(10):382-4.
[19] Balon R. Psychiatrist attitudes toward self-treatment of their own depression. Psychother Psychosom. 2007;76(5):306-10.
[20] Givens JL, Tjia J. Depressed Medical Students’ Use of Mental Health Services and Barriers to Use. Academic Medicine. 2002 Sep;77(9):918.
[21] Gupta P, Panwar N, Verma A, Debnath A. Prevalence of anxiety among medical students in a northern state of India and gaps in mental health service utilization: a cross-sectional study. The Evidence. 2025;3(1).