Psoas and Masseter Sarcopenia as Predictors of Outcome in Neurocritical Patients: A Systematic Review
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
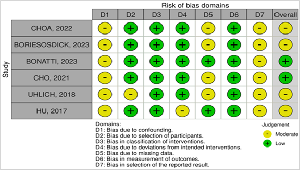
Objective: To systematically review literature on the predictive value of masseter and psoas muscle sarcopenia in neurocritical patients. Design: Systematic Review. Subjects/Patients: Adults (≥ 18 years) with traumatic brain injury and ischemic and/or hemorrhagic stroke. Methods: PRISMA-guided search of PubMed, Embase and Scopus; screening via Rayyan.ai; methodological assessment by ROBINS-I and AMSTAR2. Data included demographics, muscle areas, mortality, functional outcomes, and intensive care unit/hospital length of stay. Results: From 465 records, 6 studies (n = 962) met inclusion. Sarcopenic patients exhibited lower masseter and psoas muscle areas, correlating with higher mortality, poorer functional outcomes (Modified Rankin Scale, Glasgow Outcome Scale), and increased discharge to long-term care. Although direct length of stay data was limited, indirect measures (ventilator-free days and pneumonia rates) suggest reduced muscle mass is associated with prolonged stay. Conclusion: Masseter and psoas sarcopenia are potential predictors of adverse outcomes in neurocritical subjects. Further research is warranted to standardize sarcopenia assessment and integrate these markers into clinical risk stratification.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Isabelli Alves de Morais, Lucas Ribas Lachman, Nicolas Mikael da Silva, Helena Borges de Nadai, Maria Eduarda Beninca Taques, Victor Lisboa Ribas, Guilherme Linha Secco

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Isabelli Alves de Morais, Department of Medicine, State University of Ponta Grossa, Brazil.
Department of Medicine, State University of Ponta Grossa, Brazil.
Lucas Ribas Lachman, Department of Medicine, State University of Ponta Grossa, Brazil.
Department of Medicine, State University of Ponta Grossa, Brazil.
Nicolas Mikael da Silva, Department of Medicine, State University of Ponta Grossa, Brazil.
Department of Medicine, State University of Ponta Grossa, Brazil.
Helena Borges de Nadai, Department of Medicine, State University of Ponta Grossa, Brazil.
Department of Medicine, State University of Ponta Grossa, Brazil.
Maria Eduarda Beninca Taques, Department of Medicine, State University of Ponta Grossa, Brazil.
Department of Medicine, State University of Ponta Grossa, Brazil.
Victor Lisboa Ribas, Department of Medicine, State University of Ponta Grossa, Brazil.
Department of Medicine, State University of Ponta Grossa, Brazil.
Guilherme Linha Secco, Department of Medicine, State University of Ponta Grossa, Brazil.
Department of Medicine, State University of Ponta Grossa, Brazil.
[1] Cho HJ, Hwang Y, Yang SY, Kim M. CT anthropometric analysis of the prognosis of traumatic brain injury: A retrospective study to compare between psoas muscle and abdominal skeletal muscle. Injury. 2022 May;53(5):1652–7.
[2] Hofmeister F, Baber L, Ferrari U, Hintze S, Jarmusch S, Krause S, et al. Late-onset neuromuscular disorders in the differential diagnosis of sarcopenia. BMC Neurology. 2021 Jun 25;21(1).
[3] Byun, M. K., Cho, E. N., Chang, J., Ahn, C. M., & Kim, H. J. (2017). Sarcopenia correlates with systemic inflammation in COPD. International journal of chronic obstructive pulmonary disease, 12, 669–675. https://doi.org/10.2147/COPD.S130790
[4] Cespedes Feliciano EM, Kroenke CH, Meyerhardt JA, et al. Association of Systemic Inflammation and Sarcopenia with Survival in Nonmetastatic Colorectal Cancer: Results From the C SCANS Study. JAMA Oncol. 2017;3(12):e172319. doi:10.1001/jamaoncol.2017.2319
[5] Clement, D. S. V. M., Leerdam, M. E. V., de Jong, S., Weickert, M. O., Ramage, J. K., Tesselaar, M. E. T., & Srirajaskanthan, R. (2023). Prevalence of Sarcopenia and Impact on Survival in Patients with Metastatic Gastroenteropancreatic Neuroendocrine Tumours. Cancers, 15(3), 782. https://doi.org/10.3390/cancers15030782
[6] Wang, J. B., Xue, Z., Lu, J., He, Q. L., Zheng, Z. F., Xu, B. B., Xie, J. W., Li, P., Xu, Y., Lin, J. X., Chen, Q. Y., Cao, L. L., Lin, M., Tu, R. H., Huang, Z. N., Lin, J. L., Huang, C. M., & Zheng, C. H. (2020). Effect of sarcopenia on short- and long-term outcomes in patients with gastric neuroendocrine neoplasms after radical gastrectomy: results from a large, two-institution series. BMC cancer, 20(1), 1002. https://doi.org/10.1186/s12885-020-07506-9
[7] Hu, P., Uhlich, R., White, J., Kerby, J., & Bosarge, P. (2018). Sarcopenia Measured Using Masseter Area Predicts Early Mortality following Severe Traumatic Brain Injury. Journal of neurotrauma, 35(20), 2400–2406. https://doi.org/10.1089/neu.2017.5422
[8] Hwang, F., McGreevy, C. M., Pentakota, S. R., Verde, D., Park, J. H., Berlin, A., Glass, N. E., Livingston, D. H., & Mosenthal, A. (2019). Sarcopenia is Predictive of Functional Outcomes in Older Trauma Patients. Cureus, 11(11), e6154. https://doi.org/10.7759/cureus.6154
[9] Shibahashi, K., Sugiyama, K., Hoda, H., & Hamabe, Y. (2017). Skeletal Muscle as a Factor Contributing to Better Stratification of Older Patients with Traumatic Brain Injury: A Retrospective Cohort Study. World neurosurgery, 106, 589–594. https://doi.org/10.1016/j.wneu.2017.07.025
[10] Cho, H. J., Hwang, Y., Yang, S., & Kim, M. (2021). A Comprehensive Analysis of the Association of Psoas and Masseter Muscles with Traumatic Brain Injury Using Computed Tomography Anthropometry. Journal of Korean Neurosurgical Society, 64(6), 950–956. https://doi.org/10.3340/jkns.2021.0004
[11] Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ [Internet]. 2021 Mar 29 [cited 2025 Mar 3];372:n71. Available from: https://pubmed.ncbi.nlm.nih.gov/33782057/
[12] Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev [Internet]. 2016 Dec 5 [cited 2025 Jan 21];5(1):210. Available from: https://pubmed.ncbi.nlm.nih.gov/27919275/
[13] Sterne J A, Hernán M A, Reeves B C, Savović J, Berkman N D, Viswanathan M et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions BMJ 2016; 355: i4919 doi:10.1136/bmj.i4919
[14] Shea, B. J., Reeves, B. C., Wells, G., Thuku, M., Hamel, C., Moran, J., Moher, D., Tugwell, P., Welch, V., Kristjansson, E., & Henry, D. A. (2017). AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ (Clinical research ed.), 358, j4008. https://doi.org/10.1136/bmj.j4008
[15] Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. doi: 10.1136/bmj.n71. This work is licensed under CC BY 4.0. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/
[16] Walston JD. Sarcopenia in older adults. Curr Opin Rheumatol. 2012 Nov;24(6):623–7.
[17] Varma S, Wilson MSJ, Naik M, Sandhu A, Ota HCU, Aylwin C, et al. The associations of psoas and masseter muscles with sarcopenia and related adverse outcomes in older trauma patients: a retrospective study. Aging Clin Exp Res. 2022 Aug;34(8):1901–8.
[18] Wang Y, Li L, Pan Q, Zhong Y, Zou X. Psoas muscle morphology as a sarcopenia marker to predict outcomes of geriatric trauma patients: A systematic review and meta-analysis. Geriatr Orthop Surg Rehabil. 2023 Aug 12;14:21514593231195244.
[19] Ardeljan AD, Hurezeanu R. Sarcopenia. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025.
[20] Badminton R, Christie R, Brohi K, Cole E. Pre-injury sarcopenia and the association with discharge destination in critical care trauma patients. Trauma. 2025 Jan;27(1):57–64.
[21] Zhang, X. M., Chen, D., Xie, X. H., Zhang, J. E., Zeng, Y., & Cheng, A. S. (2021). Sarcopenia as a predictor of mortality among the critically ill in an intensive care unit: a systematic review and meta-analysis. BMC geriatrics, 21(1), 339. https://doi.org/10.1186/s12877-021-02276-w
[22] Koh, J. H., Tan, L. T. P., Lim, C. Y. J., Yuen, L. Z. H., Ho, J. S. Y., Tan, J. A., Sia, C. H., Yeo, L. L. L., Koh, F. H. X., Hallinan, J. T. P. D., Makmur, A., Tan, B. Y. Q., & Tan, L. F. (2024). Association of head and neck CT-derived sarcopenia with mortality and adverse outcomes: A systematic review. Archives of gerontology and geriatrics, 126, 105549. https://doi.org/10.1016/j.archger.2024.105549.
[23] Pisano F, Bilotta F. The predictive value of the Verbal Glasgow Coma Scale in traumatic brain injury: A systematic review. J Head Trauma Rehabil. 2024 Feb 27;39(4):273–83.
[24] Jung HN, Jung CH, Hwang YC. Sarcopenia in youth. Metabolism. 2023 Jul;144(155557):155557.
[25] Boriesosdick J, Alexey Surov, Michael A, Christoph Mönninghoff, Julius Henning Niehoff, Nina Pauline Haag, et al. Sarcopenia is a predictor of patient death in acute ischemic stroke. Journal of Stroke and Cerebrovascular Diseases. 2023 Dec 1;32(12):107421-1.
[26] Matteo Bonatti, Lombardo F, Valletta R, Comai A, Petralia B, Giacomo Avesani, et al. Myosteatosis as an independent predictor of short-term mortality in successfully reperfused acute ischemic stroke. The Neuroradiology Journal. 2022 May 4;36(1):17-22.