Early Second Trimester Serum Lipid Profile as a Predictor of Gestational Hypertension and Preeclampsia: A Prospective Hospital-Based Study
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
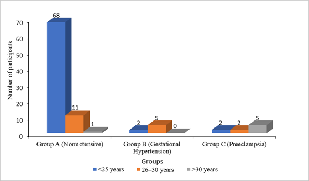
Objective: To evaluate the association between early second-trimester serum lipid concentrations and the subsequent risk of developing gestational hypertension and preeclampsia. Design: A prospective hospital-based observational study. Subjects/Patients: A total of 100 antenatal women (both primigravidae and multigravidae) with singleton pregnancies between 14 and 20 weeks of gestation who had no preexisting medical illnesses, with normal baseline blood pressure, were enrolled. Methods: Serum lipid profiles of participants were measured, and participants were followed until delivery. Based on blood pressure and proteinuria, participants were classified as normotensive, having gestational hypertension, or preeclampsia. Data were statistically analysed. Results: Among the participants, 82% antenatal women remained normotensive (Group A), 7% developed gestational hypertension (Group B), and 11% developed preeclampsia (Group C). Higher serum lipid profiles were seen in women who subsequently developed hypertensive disorders compared to normotensive women (p < 0.05). Elevated lipid levels were more pronounced in preeclamptic women, indicating an atherogenic trend with increasing disease severity. Conclusion: Overall, the study demonstrated that the association of altered lipid profiles during the early second trimester resulted in increased risk of gestational hypertension and preeclampsia. Prompt recognition of lipid screening is recommended for identifying high-risk pregnancies and enabling timely preventive interventions.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Nithya M.P.

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Nithya M.P., Senior Resident, Department of OBG, Karuna Medical College, Chittur, Kerala, India.
Senior Resident, Department of OBG, Karuna Medical College, Chittur, Kerala, India.
[1] ACOG Practice Bulletin No. 203: Chronic Hypertension in Pregnancy. Obstet Gynecol. 2019 Jan;133(1):e26–50. https://doi.org/10.1097/AOG.0000000000003025
[2] Countouris M, Mahmoud Z, Cohen JB, Crousillat D, Hameed AB, Harrington CM, et al. Hypertension in Pregnancy and Postpartum: Current Standards and Opportunities to Improve Care. Circulation. 2025 Feb 18;151(7):490–507. https://doi.org/10.1161/circulationaha.124.073302
[3] Newman C, Petruzzi V, Ramirez PT, Hobday C. Hypertensive Disorders of Pregnancy. Methodist DeBakey Cardiovasc J. 20(2):4–12. https://doi.org/10.14797/mdcvj.1305.
[4] Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. 2000 Jul;183(1):s1–22. https://doi.org/10.1067/mob.2000.107928
[5] Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin, Number 222. Obstet Gynecol. 2020 Jun;135(6):e237–60. https://doi.org/10.1097/AOG.0000000000003891
[6] Shaw LJ, Patel K, Lala-Trindade A, Feltovich H, Vieira L, Kontorovich A, et al. Pathophysiology of Preeclampsia-Induced Vascular Dysfunction and Implications for Subclinical Myocardial Damage and Heart Failure. JACC Adv. 2024 Jun;3(6):100980. https://doi.org/10.1016/j.jacadv.2024.100980
[7] Preda A, Preda SD, Mota M, Iliescu DG, Zorila LG, Comanescu AC, et al. Dyslipidemia in Pregnancy: A Systematic Review of Molecular Alterations and Clinical Implications. Biomedicines. 2024 Oct 3;12(10):2252. https://doi.org/10.3390/biomedicines12102252
[8] Lewek J, Bielecka-Dąbrowa A, Toth PP, Banach M. Dyslipidaemia management in pregnant patients: a 2024 update. Eur Heart J Open. 2024 Apr 26;4(3): oeae032. https://doi.org/10.1093/ehjopen/oeae032
[9] Qin X, Ai F, Zhou Q, Zhang Y, Yan X. Pre-eclampsia, gestational hypertension, and lipid levels during pregnancy: a systematic review and meta-analysis. Arch Gynecol Obstet. 2025;312(2):385–402. https://doi.org/10.1007/s00404-025-07955-5
[10] Mulder JWCM, Kusters DM, Roeters van Lennep JE, Hutten BA. Lipid metabolism during pregnancy: consequences for mother and child. Curr Opin Lipidol. 2024 Jun;35(3):133. https://doi.org/10.1097/MOL.0000000000000958
[11] Hart NR. Paradoxes: Cholesterol and Hypoxia in Preeclampsia. Biomolecules. 2024 Jun;14(6):691. https://doi.org/10.3390/biom14060691
[12] Kalapouti E, Bothou A, Harizopoulou V, Vlachou M, Vasilili Zampeli M, Diamanti A. Lipidomic Signatures in Maternal Blood and Placenta: Systematic Evidence Linking Lipid Profiles to Pregnancy Outcomes and Fetal Growth. Metab Open. 2025 Sep 24;100398. https://doi.org/10.1016/j.metop.2025.100398
[13] Bartho LA, Keenan E, Walker SP, MacDonald TM, Nijagal B, Tong S, et al. Plasma lipids are dysregulated preceding diagnosis of preeclampsia or delivery of a growth restricted infant. eBioMedicine. 2023 Aug; 94:104704. https://doi.org/10.1016/j.ebiom.2023.104704
[14] Roberts WC. The Friedewald-Levy-Fredrickson formula for calculating low-density lipoprotein cholesterol, the basis for lipid-lowering therapy. Am J Cardiol. 1988 Aug;62(4):345–6. https://doi.org/10.1016/0002-9149(88)90248-2
[15] Wang A, Rana S, Karumanchi SA. Preeclampsia: the role of angiogenic factors in its pathogenesis. Physiol Bethesda Md. 2009 Jun; 24:147–58. https://doi.org/10.1152/physiol.00043.2008
[16] Qin X, Ai F, Zhou Q, Zhang Y, Yan X. Pre-eclampsia, gestational hypertension, and lipid levels during pregnancy: a systematic review and meta-analysis. Arch Gynecol Obstet. 2025 May 23;312(2):385–402. https://doi.org/10.1007/s00404-025-08052-0
[17] Duckitt K, Harrington D. Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. BMJ. 2005 Mar 12;330(7491):565. https://doi.org/10.1136/bmj.38380.674340.e0
[18] Stekkinger E, Scholten R, van der Vlugt M, van Dijk A, Janssen M, Spaanderman M. Metabolic syndrome and the risk for recurrent pre-eclampsia: a retrospective cohort study. BJOG Int J Obstet Gynaecol. 2013;120(8):979–86. https://doi.org/10.1111/1471-0528.12189
[19] McElwain CJ, Tuboly E, McCarthy FP, McCarthy CM. Mechanisms of Endothelial Dysfunction in Pre-eclampsia and Gestational Diabetes Mellitus: Windows into Future Cardiometabolic Health? Front Endocrinol. 2020; 11:655. https://doi.org/10.3389/fendo.2020.00655
[20] Mao J, Sun H, Shen Q, Zou C, Yang Y, Du Q. Impact of pre-pregnancy body mass index on preeclampsia. Front Med. 2025 Feb 5; 12:1529966. https://doi.org/10.3389/fmed.2025.1529966
[21] Qin X, Ai F, Zhou Q, Zhang Y, Yan X. Pre-eclampsia, gestational hypertension, and lipid levels during pregnancy: a systematic review and meta-analysis. Arch Gynecol Obstet. 2025 Aug 1;312(2):385–402. https://doi.org/10.1007/s00404-025-08052-0
[22] Stadler JT, Scharnagl H, Wadsack C, Marsche G. Preeclampsia Affects Lipid Metabolism and HDL Function in Mothers and Their Offspring. Antioxidants. 2023 Mar 24;12(4):795. https://doi.org/10.3390/antiox12040795
[23] Rashidian P, Parsaei M, Hantoushzadeh S, Salmanian B. Investigating the association of albuminuria with the incidence of preeclampsia and its predictive capabilities: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2025 Mar 20;25(1):322. https://doi.org/10.1186/s12884-025-07444-z