Hesitation and Acceptance of Vaccines Among Students of Health Colleges in the Tabuk Area: Have The COVID-19 Pandemic and Vaccinations Efforts Aggravated the Issue?
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
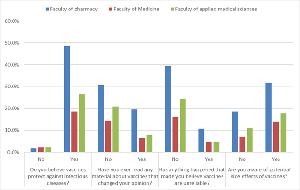
Introduction: Vaccines are one of the pillars of the current medical care worldwide. COVID19 pandemic and the subsequent vaccinations campaigns had a complex impact on vaccine hesitancy. In this study we aimed to explore the level of hesitation and acceptance of vaccines among the medical students at the University of Tabuk. Methods: This is a questionnaire based cross sectional study. The questionnaire was available online for data collection in the time period from October 20 2023 to 31 March 2024. Results: Students from a wide range of medical specialties participated in this study. Although most of the students (93.5%) believed that vaccines are protective some potential barriers have been identified and included insufficiency of information, and believes in conspiracy. There is increasing mistrust in the vaccines manufacturers as 27.9% of the participants agreed to this notion. Large number of the students (39.4%) said they know families that do not vaccinate their kids. A 34% of all participants acknowledged that following the pandemic, they became skeptical about getting vaccinations. Conclusion: Negative views among medical students can compromise patient care. We must equip students with skills that help them identify misinformation and ability to convey it to their surroundings and to the patients.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Rehab Ahmed, Ohod S Alshehri, Shroog F Alshammari, Kadi M Alharbi, Kadi M Alharbi, Ehab Ahmed Frah, Nehal Elsherbiny

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Ohod S Alshehri, PharmD Program, Faculty of Pharmacy, University of Tabuk, Tabuk, Saudi Arabia.
PharmD Program, Faculty of Pharmacy, University of Tabuk, Tabuk, Saudi Arabia.
Shroog F Alshammari, PharmD Program, Faculty of Pharmacy, University of Tabuk, Tabuk, Saudi Arabia.
PharmD Program, Faculty of Pharmacy, University of Tabuk, Tabuk, Saudi Arabia.
Kadi M Alharbi, PharmD Program, Faculty of Pharmacy, University of Tabuk, Tabuk, Saudi Arabia.
PharmD Program, Faculty of Pharmacy, University of Tabuk, Tabuk, Saudi Arabia.
Ehab Ahmed Frah, Statistics Department, Faculty of Science, University of Tabuk, Tabuk, Saudi Arabia.
Statistics Department, Faculty of Science, University of Tabuk, Tabuk, Saudi Arabia.
Nehal Elsherbiny, Department of Pharmaceutical Chemistry, Faculty of Pharmacy, University of Tabuk, Tabuk, Saudi Arabia.
Department of Pharmaceutical Chemistry, Faculty of Pharmacy, University of Tabuk, Tabuk, Saudi Arabia.
[1] Ugboko HU, Nwinyi OC, Oranusi SU, et al. Childhood diarrhoeal diseases in developing countries. Heliyon 2020;6:e03690. https://doi.org/10.1016/J.HELIYON.2020.E03690.
[2] Balloux F, van Dorp L. Q&A: What are pathogens, and what have they done to and for us? BMC Biol 2017;15:1–6. https://doi.org/10.1186/S12915-017-0433-Z/FIGURES/1.
[3] Murray CJ, Ikuta KS, Sharara F, et al. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. The Lancet 2022;399:629–55. https://doi.org/10.1016/S0140-6736(21)02724-0.
[4] Verket M, Jacobsen M, Schütt K, et al. Influenza vaccination in patients affected by diabetes. Eur Heart J Suppl 2023;25: A36–41. https://doi.org/10.1093/EURHEARTJSUPP/SUAC119.
[5] Alghamdi S. The role of vaccines in combating antimicrobial resistance (AMR) bacteria. Saudi J Biol Sci 2021;28:7505–10. https://doi.org/10.1016/J.SJBS.2021.08.054.
[6] Michel JP, Frangos E. The Implications of Vaccines in Older Populations. Vaccines (Basel) 2022;10. https://doi.org/10.3390/VACCINES10030431.
[7] Suryadevara M. Vaccine-Preventable Disease Outbreaks. Vaccines (Basel) 2021:419–39. https://doi.org/10.1007/978-3-030-58414-6_36.
[8] Baldwin AS, Tiro JA, Zimet GD. Broad perspectives in understanding vaccine hesitancy and vaccine confidence: an introduction to the special issue. J Behav Med 2023;46:1–8. https://doi.org/10.1007/S10865-023-00397-8.
[9] Orenstein WA, Gellin BG, Beigi RH, et al. A Call for Greater Consideration for the Role of Vaccines in National Strategies to Combat Antibiotic-Resistant Bacteria: Recommendations from the National Vaccine Advisory Committee: Approved by the National Vaccine Advisory Committee on June 10, 2015. Public Health Reports 2016;131:11. https://doi.org/10.1177/003335491613100105.
[10] Roy DN, Biswas M, Islam E, et al. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: A systematic review. PLoS One 2022;17. https://doi.org/10.1371/JOURNAL.PONE.0265496.
[11] Majid U, Ahmad M, Zain S, et al. COVID-19 vaccine hesitancy and acceptance: a comprehensive scoping review of global literature. Health Promot Int 2022;37. https://doi.org/10.1093/HEAPRO/DAAC078.
[12] Zhang L, Wang W, Wang S. Effect of Vaccine Administration Modality on Immunogenicity and Efficacy. Expert Rev Vaccines 2015;14:1509. https://doi.org/10.1586/14760584.2015.1081067.
[13] Wang S, Ren W, Zhang B, et al. Knowledge, Attitude, and Uptake of Human Papillomavirus (HPV) Vaccination among Chinese Female Adults: A National Cross-sectional Web-Based Survey Based on a Large E-commerce Platform. Matern Child Health J 2024;28:746–57. https://doi.org/10.1007/S10995-023-03888-X.
[14] Shen Y, Wang J, zhao Q, et al. Predicting future vaccination habits: The link between influenza vaccination patterns and future vaccination decisions among old aged adults in China. J Infect Public Health 2024;17:1079–85. https://doi.org/10.1016/J.JIPH.2024.04.017.
[15] Lau BHP, Yuen SWH, Yue RPH, et al. Understanding the societal factors of vaccine acceptance and hesitancy: evidence from Hong Kong. Public Health 2022;207:39–45. https://doi.org/10.1016/J.PUHE.2022.03.013.
[16] Begum T, Efstathiou N, Bailey C, et al. Cultural and social attitudes towards COVID-19 vaccination and factors associated with vaccine acceptance in adults across the globe: A systematic review. Vaccine 2024;42. https://doi.org/10.1016/J.VACCINE.2024.05.041.
[17] Alshurman BA, Khan AF, Mac C, et al. What Demographic, Social, and Contextual Factors Influence the Intention to Use COVID-19 Vaccines: A Scoping Review. Int J Environ Res Public Health 2021;18. https://doi.org/10.3390/IJERPH18179342.
[18] Nuwarda RF, Ramzan I, Weekes L, et al. Vaccine Hesitancy: Contemporary Issues and Historical Background. Vaccines (Basel) 2022;10. https://doi.org/10.3390/VACCINES10101595.
[19] Puri N, Coomes EA, Haghbayan H, et al. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother 2020; 16:2586–93. https://doi.org/10.1080/21645515.2020.1780846.
[20] Terry K, Yang F, Yao Q, et al. The role of social media in public health crises caused by infectious disease: a scoping review. BMJ Glob Health 2023;8. https://doi.org/10.1136/BMJGH-2023-013515.
[21] Omar A, Gul I, Ali I. Exploring vaccine hesitancy and acceptance in the general population of Pakistan: Insights into COVID-19-related distress, risk perception, and stigma. Hum Vaccin Immunother 2024;20. https://doi.org/10.1080/21645515.2024.2309699.
[22] Cascini F, Pantovic A, Al-Ajlouni Y, et al. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. E Clinical Medicine 2021;40. https://doi.org/10.1016/J.ECLINM.2021.101113.
[23] Elliott TR, Perrin PB, Powers MB, et al. Predictors of Vaccine Hesitancy among Health Care Workers during the COVID-19 Pandemic. Int J Environ Res Public Health 2022;19. https://doi.org/10.3390/IJERPH19127123.
[24] Paris C, Bénézit F, Geslin M, et al. COVID-19 vaccine hesitancy among healthcare workers. Infect Dis Now 2021;51:484–7. https://doi.org/10.1016/J.IDNOW.2021.04.001.
[25] Peterson CJ, Lee B, Nugent K. COVID-19 Vaccination Hesitancy among Healthcare Workers-A Review. Vaccines (Basel) 2022;10. https://doi.org/10.3390/VACCINES10060948.
[26] Albarakati R, Almatrafi L, Fatta G, et al. Investigating Factors Associated with Vaccine Hesitancy in Makkah, KSA. World J Vaccines 2019;9:37–48. https://doi.org/10.4236/WJV.2019.92003.
[27] Galagali PM, Kinikar AA, Kumar VS. Vaccine Hesitancy: Obstacles and Challenges. Curr Pediatr Rep 2022;10:241. https://doi.org/10.1007/S40124-022-00278-9.
[28] McCready JL, Nichol B, Steen M, et al. Understanding the barriers and facilitators of vaccine hesitancy towards the COVID-19 vaccine in healthcare workers and healthcare students worldwide: An Umbrella Review. PLoS One 2023;18:e0280439. https://doi.org/10.1371/JOURNAL.PONE.0280439.
[29] Yang Z, Luo X, Jia H. Is It All a Conspiracy? Conspiracy Theories and People’s Attitude to COVID-19 Vaccination. Vaccines (Basel) 2021; 9:1051. https://doi.org/10.3390/VACCINES9101051.
[30] Sojati J, Murali A, Rapsinski G, et al. Do Not Throw Away Your Shot: Pilot Study in Improving Medical School Curricula Through Focused Vaccine Education. AJPM Focus 2023; 3:100178. https://doi.org/10.1016/J.FOCUS.2023.100178.
[31] Gautier S, Hammarlin MM, Paulik E, et al. New pedagogical tools for vaccine education: preparing future healthcare workers for the next pandemic. BMC Med Educ 2024;24:1-6. https://doi.org/10.1186/S12909-024-06274-5/TABLES/1.
[32] Aldajani FN, Aldosari M. Pharmacist-led vaccination services in the Middle East. J Pharm Policy Pract 2023;16:1-6. https://doi.org/10.1186/S40545-023-00664-8/TABLES/1.
[33] Alrasheedy AA, Alharbi AT, Alturaifi HA, et al. Community pharmacists’ knowledge, beliefs, and perceived barriers toward vaccination services at community pharmacies: A cross-sectional study from Saudi Arabia. Hum Vaccin Immunother 2024; 20:2414551. https://doi.org/10.1080/21645515.2024.2414551.
[34] Meraya AM, Syed MH, Shabi AA, et al. Assessment of community pharmacists’ knowledge, attitudes and their willingness to provide vaccination services in Saudi Arabia. PLoS One 2024;19:e0304287. https://doi.org/10.1371/JOURNAL.PONE.0304287.
[35] WHO Immunization Data portal - Eastern Mediterranean Region n.d. https://immunizationdata.who.int/dashboard/regions/eastern-mediterranean-region/SAU (accessed February 26, 2025).
[36] Bin Alamir AA. Childhood vaccination hesitancy in Saudi Arabia: are we still facing a problem? Saudi Med J 2024;45:551-9. https://doi.org/10.15537/SMJ.2024.45.6.20240116.
[37] Vanderslott S, Enria L, Bowmer A, et al. Attributing public ignorance in vaccination narratives. Soc Sci Med 2022;307. https://doi.org/10.1016/J.SOCSCIMED.2022.115152.
[38] Fuławka K, Hertwig R, Pachur T. COVID-19 vaccine refusal is driven by deliberate ignorance and cognitive distortions. NPJ Vaccines 2024;9:167. https://doi.org/10.1038/S41541-024-00951-8.