Comparison of Rapid Acute Physiological Score (RAPS) with Modified Rapid Emergency Medicine Score (mREMS) in Prediction of Mortality in Traumatic Injury Patients Presenting to Emergency Medicine Department: A Prospective Observational Study
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
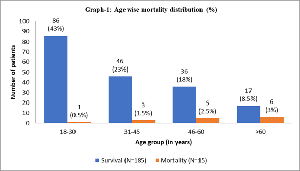
Objective: This study aims to assess and compare the prognostic value of Rapid Acute Physiological Score and modified Rapid Emergency Medicine Score for mortality and outcome of trauma patients presenting in Emergency department. Methods: This prospective observational study was conducted among patients > 18 years age presenting with traumatic injury at B J Medical College. The RAPS and mREMS were calculated. The efficacy in predicting mortality was evaluated using ROC curve analysis. Results: In the 200 patients studied (68% males) 43.5% were in 18-30 years age group. Mortality rate was 7.50% (n = 15), also found that among 15 non-survivors, 93.33% each had RAPS >6 and mREMS >8. Sensitivity, specificity, positive predictive value and negative predictive value of RAPS and mREMS for mortality were 93.33%, 96.75%, 70%, 99.44% and 99.92%, 93.51%, 55.55% and 99.97% (p<0.0001) respectively. ROC curve for RAPS and mREMS score was 0.981 and 0.995 respectively, showed no significant difference (p=0.143), but mREMS was slightly superior to RAPS in predicting mortality. Conclusion: We found that mREMS score is comparable to RAPS and marginally superior in predicting death and vegetative state. We also found that mREMS score is rather better predictor of severe disability (morbidity) than RAPS in trauma.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Shruti V. Sangani, MD, Vishakhaben G. Patel, MD, Sonal K. Ginoya, MD

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Shruti V. Sangani, MD, Associate Professor, Department of Emergency Medicine, B. J. Medical College, Civil Hospital, Asarwa, Ahmedabad, Gujarat, India.
Associate Professor, Department of Emergency Medicine, B. J. Medical College, Civil Hospital, Asarwa, Ahmedabad, Gujarat, India.
Vishakhaben G. Patel, MD, Senior Resident, Department of Emergency Medicine, Government Medical College, Vadodara, Gujarat, India. Past Affiliation: 3rd year Resident, Department of Emergency Medicine, B. J. Medical College, Civil Hospital, Asarwa, Ahmedabad, Gujarat, India.
Senior Resident, Department of Emergency Medicine, Government Medical College, Vadodara, Gujarat, India.
Past Affiliation: 3rd year Resident, Department of Emergency Medicine, B. J. Medical College, Civil Hospital, Asarwa, Ahmedabad, Gujarat, India.
Sonal K. Ginoya, MD, Assistant Professor, Department of Emergency Medicine, B. J. Medical College, Civil Hospital, Asarwa, Ahmedabad, Gujarat, India.
Assistant Professor, Department of Emergency Medicine, B. J. Medical College, Civil Hospital, Asarwa, Ahmedabad, Gujarat, India.
[1] WHO. Global report on injuries and violence. 19 June 2024.
[2] Indian Society for Trauma & Acute Care. Trauma in India. Available from: https://traumaindia.org
[3] Rhee P, Joseph B, Pandit V, Aziz H, Vercruysse G, Kolvatunyou N, Friese RS. Increasing trauma deaths in the United States. Ann Surg. 2014 Jul;260(1):13-21.
[4] Velopulos CG, Enwerem NY, Obirieze A, Hui X, Hashmi ZG, Scott VK, Cornwell EE III, Schneider EB, Haider AH. National cost of trauma care by payer status. J Surg Res. 2013 Sep;184(1):444-9.
[5] Shortell SM, Zimmerman JE, Rousseau DM, Gillies RR, Wagner DP, Draper EA, et al. The performance of intensive care units: does good management make a difference? Med Care. 1994 May;32(5):508-25.
[6] MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366-378.
[7] Perel P, Prieto-Merino D, Shakur H, Clayton T, Lecky F, Bouamra O, et al. Predicting early death in patients with traumatic bleeding: development and validation of prognostic model. BMJ. 2012;345:e5166.
[8] Demetriades D, Kimbrell B, Salim A, Velmahos G, Rhee P, Preston C, et al. Trauma deaths in a mature urban trauma system: is "trimodal" distribution a valid concept? J Am Coll Surg. 2005;201(3):343-348.
[9] Demetriades D, Murray J, Charalambides K, Alo K, Velmahos G, Rhee P, et al. Trauma fatalities: time and location of hospital deaths. J Am Coll Surg. 2004;198(1):20-26.
[10] De Souza Nouguiera L, de Alancar Domingues C, Poggetti RS, de Souse RMC. Nursing workload in intensive care unit trauma patients: analysis of associated factors. Plus One. 2014;9(11):e112125.
[11] Kumagai G, Tsoulfas P, Toh S, McNiece I, Bramlett HM, Dietrich WD. Genetically modified mesenchymal stem cells (MSC) promote axonal regeneration and prevent hypersensitivity after spinal cord injury. Exp Neurol. 2013;248:369-380.
[12] Trunkey DD, Siegel J, Baker S, et al. Panel: current status of trauma severity indices. J Trauma. 1983;23:185-191.
[13] Civil ID, Schwab CW. Clinical prospective injury severity scoring: when is it accurate? J Trauma. 1989;29:613-619.
[14] Goldberg JL, Goldberg J, Levy PS, et al. Measuring the severity of injury: the validity of the revised estimated survival probability index. J Trauma. 1984;24:420-426.
[15] Sartorius D, Le Manach Y, David JS, Rancurel E, Smail N, Thicoipe M, et al. Mechanism, Glasgow coma scale, age, and arterial pressure (MGAP): a new simple prehospital triage score to predict mortality in trauma patients. Crit Care Med. 2010;38(3):831-7.
[16] Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818-29.
[17] Olsson T, Terent A, Lind L. Rapid emergency medicine score: a new prognostic index for in-hospital mortality in non-surgical emergency department patients. J Intern Med. 2004;255:579-87.
[18] Eid HO, Abu-Zidan FM. New injury severity score is a better predictor of mortality for blunt trauma patients than the injury severity score. World J Surg. 2015;39:165-71.
[19] Imhoff BF, Thompson NJ, Hastings MA, Nazir N, Moncure M, Cannon CM. Rapid emergency medicine score (REMS) in the trauma population: a retrospective study. BMJ Open. 2014;4:e004738.
[20] Ha DT, Dang TQ, Tran NV, Vo NY, Nguyen ND, Nguyen TV. Prognostic performance of the Rapid Emergency Medicine Score (REMS) and Worthing Physiological Scoring system (WPS) in emergency department. Int J Emerg Med. 2015;8(1):18.
[21] Rhee K, Fisher C, Willitis N. The rapid acute physiology score. Am J Emerg Med. 1987;5(4):278-86.
[22] Imhoff BE, Thompson NJ, Hastings MA, Nazir N, Moncure M, Cannon CM. Rapid emergency medicine score (REMS) in trauma population: a retrospective study. Am J Emerg Med. 2017;4:423-9.
[23] Olsson T, Lind L. Comparison of the rapid emergency medicine score and APACHE II in nonsurgical emergency department patients. Acad Emerg Med. 2003;10(10):1040-8.
[24] Miller RT, Nazir N, McDonald T, Cannon CM. The modified rapid emergency medicine score: A novel trauma triage tool to predict in-hospital mortality. Am J Emerg Med. 2017;35(1):97-101.
[25] Nakhjavan-Shahraki B, Baikpour M, Yousefifard M, Nikseresht ZS, Abiri S, Razaz JM, et al. Rapid acute physiology score versus rapid emergency medicine score in trauma outcome prediction: a comparative study. Emerg. 2017;5(1).
[26] Park HO, Kim JW, Kim SH, Moon SH, Byun JH, Kim KN, et al. Usability verification of the Emergency Trauma Score (EMTRAS) and Rapid Emergency Medicine Score (REMS) in patients with trauma: a retrospective cohort study. Medicine (Baltimore). 2017;96(44):e8375.
[27] Alireza Ala, Samad Shams Vahdati, Mahsa Jalali, Sina Parsay. Rapid emergency medicine score (REMS) as a predictive value for 30-day outcome of non-surgical patients referred to emergency department. Indian journal of critical care medicine (2020):10.5005/jp-journals-10071-23456
[28] Garkaz O, Rezazadeh F, Golfiroozi S, et al. Predicting the 28-Day Mortality of Non-Trauma Patients using REMS and RAPS; a Prognostic Accuracy Study. Arch Acad Emerg Med. 2022;10(1):e52. doi:10.22037/aaem.v10i1.1601.