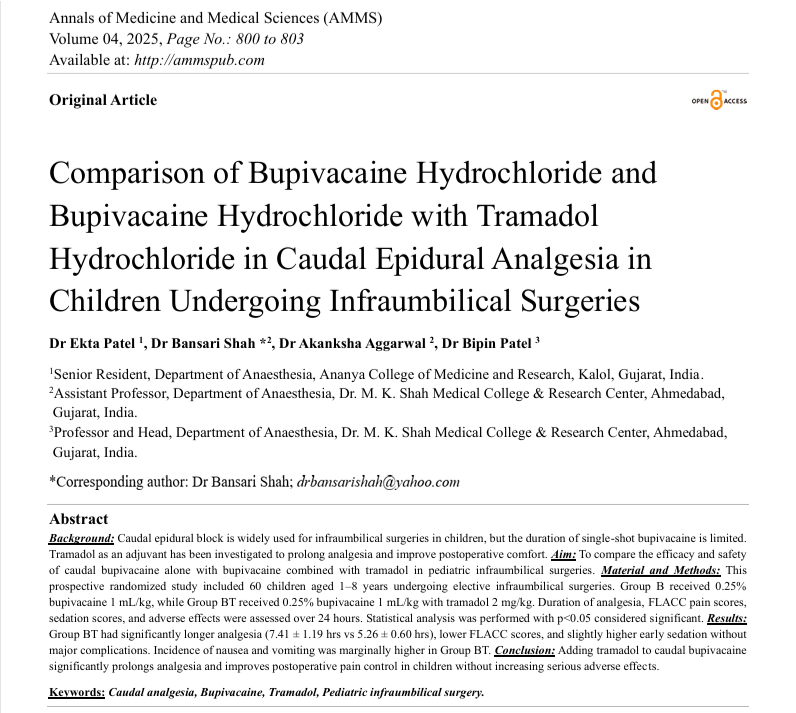
Comparison of Bupivacaine Hydrochloride and Bupivacaine Hydrochloride with Tramadol Hydrochloride in Caudal Epidural Analgesia in Children Undergoing Infraumbilical Surgeries
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
Background: Caudal epidural block is widely used for infraumbilical surgeries in children, but the duration of single-shot bupivacaine is limited. Tramadol as an adjuvant has been investigated to prolong analgesia and improve postoperative comfort. Aim: To compare the efficacy and safety of caudal bupivacaine alone with bupivacaine combined with tramadol in pediatric infraumbilical surgeries. Material and Methods: This prospective randomized study included 60 children aged 1–8 years undergoing elective infraumbilical surgeries. Group B received 0.25% bupivacaine 1 mL/kg, while Group BT received 0.25% bupivacaine 1 mL/kg with tramadol 2 mg/kg. Duration of analgesia, FLACC pain scores, sedation scores, and adverse effects were assessed over 24 hours. Statistical analysis was performed with p<0.05 considered significant. Results: Group BT had significantly longer analgesia (7.41 ± 1.19 hrs vs 5.26 ± 0.60 hrs), lower FLACC scores, and slightly higher early sedation without major complications. Incidence of nausea and vomiting was marginally higher in Group BT. Conclusion: Adding tramadol to caudal bupivacaine significantly prolongs analgesia and improves postoperative pain control in children without increasing serious adverse effects.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dr Ekta Patel, Dr Bansari Shah, Dr Akanksha Aggarwal, Dr Bipin Patel

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Dr Ekta Patel, Senior Resident, Department of Anaesthesia, Ananya College of Medicine and Research, Kalol, Gujarat, India.
Senior Resident, Department of Anaesthesia, Ananya College of Medicine and Research, Kalol, Gujarat, India.
Dr Bansari Shah, Assistant Professor, Department of Anaesthesia, Dr. M. K. Shah Medical College & Research Center, Ahmedabad, Gujarat, India.
Assistant Professor, Department of Anaesthesia, Dr. M. K. Shah Medical College & Research Center, Ahmedabad, Gujarat, India.
Dr Akanksha Aggarwal, Assistant Professor, Department of Anaesthesia, Dr. M. K. Shah Medical College & Research Center, Ahmedabad, Gujarat, India.
Assistant Professor, Department of Anaesthesia, Dr. M. K. Shah Medical College & Research Center, Ahmedabad, Gujarat, India.
Dr Bipin Patel, Professor and Head, Department of Anaesthesia, Dr. M. K. Shah Medical College & Research Center, Ahmedabad, Gujarat, India.
Professor and Head, Department of Anaesthesia, Dr. M. K. Shah Medical College & Research Center, Ahmedabad, Gujarat, India.
[1] Kokki H. Current management of pediatric postoperative pain. Expert Rev Clin Pharmacol. 2019;12(2):105-114.
[2] Suresh S, Ecoffey C, Bosenberg A, et al. The European Society of Regional Anaesthesia and Pain Therapy and the American Society of Regional Anesthesia and Pain Medicine joint committee practice advisory on pediatric regional anesthesia. Reg Anesth Pain Med. 2018;43(3):211-217.
[3] Verghese ST, Hannallah RS. Acute pain management in children. J Pain Res. 2010; 3:105-123.
[4] Polaner DM, Taenzer AH, Walker BJ, et al. Pediatric Regional Anesthesia Network (PRAN): a multi-institutional study of the use and incidence of complications of pediatric regional anesthesia. Anesth Analg. 2012;115(6):1353-1364.
[5] Ivani G, Suresh S. Caudal anesthesia and analgesia techniques in children. Curr Opin Anaesthesiol. 2017;30(5):652-657.
[6] Ecoffey C. Pediatric regional anesthesia-update. Curr Opin Anaesthesiol. 2018;31(5):674-680.
[7] Constant I, Gall O, Ecoffey C. Anaesthesia for paediatric surgery. Br J Anaesth. 2013;111(Suppl 1):i95-i105.
[8] Khalil S, Campos S, Farag E. Caudal analgesia in children: review of adjuvants and complications. Curr Opin Anaesthesiol. 2019;32(6):701-707.
[9] Gupta S, Sharma R, Singh S. Comparative study of caudal tramadol and bupivacaine versus bupivacaine alone in paediatric patients. Indian J Anaesth. 2011;55(2):118-123.
[10] Singh J, Jafra A, Anand LK. Caudal tramadol with bupivacaine for postoperative analgesia in children: a randomized controlled study. J Anaesthesiol Clin Pharmacol. 2013;29(3):303-307.
[11] Senel AC, Akyol A, Aydin ON, et al. Caudal bupivacaine-tramadol combination for postoperative analgesia in children: a randomized, double-blind, prospective study. Paediatr Anaesth. 2011;21(5):530-535.
[12] Prosser DP, Davis A, Booker PD, et al. Caudal tramadol for postoperative analgesia in paediatric patients: a comparison with bupivacaine. Paediatr Anaesth. 1997;7(6):451-454.
[13] Kumari A, Jain S, Sinha R, et al. A comparative study of caudal tramadol and bupivacaine with bupivacaine alone in children for postoperative analgesia. Anaesth Pain Intensive Care. 2015;19(3):283-287.
[14] Jindal P, Khurana G, Bansal R, et al. Caudal tramadol-bupivacaine combination versus bupivacaine alone in children: analgesic efficacy and safety. J Clin Diagn Res. 2016;10(7): UC09-UC12.
[15] Verghese S, Hannallah R, Long J, et al. Adverse effects of caudal adjuvants in children: a systematic review and meta-analysis. Anesth Analg. 2017;124(6):1940-1951.