Vulvar Cancers and Precancerous Lesions - Surgical Management with Reconstructive Strategies: A Case Series of 4 Patients
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
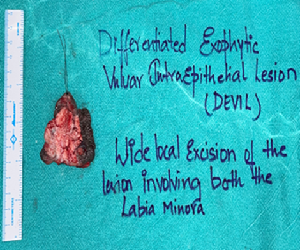
Vulvar cancer constitutes 5% of the malignancies of the female genital tract and 95% of the vulvar cancers are squamous cell carcinoma, followed by melanoma, sarcoma and basalioma. Pruritus is the most common and long-lasting reported symptom of vulvar cancer, followed by vulvar bleeding, discharge, dysuria, and pain. Diagnosis is confirmed by biopsy. The gold standard treatment of vulvar cancer is radical vulvectomy, with wide local excison of the lesion ensuring clearing margins along with enbloc resection of the inguinal lymph nodes. Vulvar intraepithelial neoplasia is a non-invasive squamous lesion, a precursor of vulvar squamous cell cancer. Clinically vulvar precancerous lesions may be flat, elevated, papulated or raised with the presence of ulcers or erosions. A thorough examination of the vulva, perineum, perianal, and anal regions, including the cervix and vagina, is essential to look for multicentricity. A good biopsy from the suspicious areas is confirmatory of diagnosis, and multiple punch biopsies should be performed for large, multicentric, and multi-colored lesions. Excisonal surgery is the treatment of choice for vulvar precancerous lesions of any type. we report 4 cases of vulvar lesions, 2 of which are vulvar cancer and two precancerous lesions of the vulva which we have diagnosed and treated in our center.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dr Nagendra Parvataneni, Dr Amulya Chiliki, Dr Hemanth N, Dr Madhavi M, Dr Mahesh Chejarla, Dr Reshma G, Dr Indrani Biswas

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Dr Nagendra Parvataneni, Senior Consultant and Head of the Department, Surgical Oncology, KIMS, Secunderabad, Telangana, India.
Senior Consultant and Head of the Department, Surgical Oncology, KIMS, Secunderabad, Telangana, India.
Dr Hemanth N, Senior Consultant, Department of Plastic Surgery and Reconstructive Surgery, KIMS, Secunderabad, Telangana, India.
Senior Consultant, Department of Plastic Surgery and Reconstructive Surgery, KIMS, Secunderabad, Telangana, India.
Dr Madhavi M, Senior Consultant, Department of obstetrics and Gynaecology, KIMS, Secunderabad, Telangana, India.
Senior Consultant, Department of obstetrics and Gynaecology, KIMS, Secunderabad, Telangana, India.
Dr Mahesh Chejarla, Senior Resident, Surgical Oncology, KIMS, Secunderabad, Telangana, India.
Senior Resident, Surgical Oncology, KIMS, Secunderabad, Telangana, India.
Dr Reshma G, Senior Resident, Surgical Oncology, KIMS, Secunderabad, Telangana, India.
Senior Resident, Surgical Oncology, KIMS, Secunderabad, Telangana, India.
Dr Indrani Biswas, Physician Assistant, Surgical Oncology, KIMS, Secunderabad, Telangana, India.
Physician Assistant, Surgical Oncology, KIMS, Secunderabad, Telangana, India.
[1] Alkatout I, Schubert M, Garbrecht N, et al. Vulvar cancer: epidemiology, clinical presentation, and management options. Int J Womens Health. 2015; 7:305-313. Published 2015 Mar 20. doi:10.2147/IJWH.S68979
[2] Rakislova N, Clavero O, Alemany L, et al. Histological characteristics of HPV-associated and -independent squamous cell carcinomas of the vulva: a study of 1,594 cases. Int J Cancer. 2017; 141: 2517-2527.
[3] Lin G, Chen CY, Liu FY, et al. Computed tomography, magnetic resonance imaging and FDG positron emission tomography in the management of vulvar malignancies. Eur Radiol. 2015; 25: 1267-1278.
[4] Yap J, O'Neill D, Nagenthiran S, Dawson CW, Luesley DM. Current insights into the aetiology, pathobiology, and management of local disease recurrence in squamous cell carcinoma of the vulva. BJOG. 2017; 124: 946-954.
[5] Hacker NF, Eifel PJ, van der Velden J. Cancer of the vulva. Int J Gynecol Obstet. 2015; 131(Suppl 2): S76-83.
[6] Tock S, Wallet J, Belhadia M, et al. Outcomes of the use of different vulvar flaps for reconstruction during surgery for vulvar cancer. Eur J Surg Oncol. 2019; 45: 1625-1631.
[7] Koh W-J, Greer BE, Abu-Rustum NR, et al. Vulvar cancer, version 1.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2017; 15: 92-120.
[8] Stehman FB, Bundy BN, Dvoretsky PM, Creasman WT. Early stage I carcinoma of the vulva treated with ipsilateral superficial inguinal lymphadenectomy and modified radical hemivulvectomy: a prospective study of the Gynecologic Oncology Group. Obstet Gynecol. 1992; 79: 490-497.
[9] Katz A, Eifel PJ, Jhingran A, Levenback CF. The role of radiation therapy in preventing regional recurrences of invasive squamous cell carcinoma of the vulva. Int J Radiat Oncol Biol Phys. 2003; 57: 409-418.
[10] Tehman FB, Bundy BN, Thomas G, et al. Groin dissection versus groin radiation in carcinoma of the vulva: a Gynecologic Oncology Group study. Int J Radiat Oncol Biol Phys. 1992; 24: 389-396.
[11] Stehman FB, Look KY. Carcinoma of the vulva. Obstet Gynecol. 2006; 107: 719-733.
[12] Van der Zee AGJ, Oonk MH, De Hullu JA, et al. Sentinel node dissection is safe in the treatment of early-stage vulvar cancer. J Clin Oncol. 2008; 26: 884-889.
[13] Covens A, Vella ET, Kennedy EB, Reade CJ, Jimenez W, Le T. Sentinel lymph node biopsy in vulvar cancer: systematic review, meta-analysis and guideline recommendations. Gynecol Oncol. 2015; 137: 351-361.
[14] Hacker NF, Eifel PJ, van der Velden J. Cancer of the vulva. Int J Gynecol Obstet. 2015; 131(Suppl 2): S76-83.
[15] Gaffney DK, King B, Viswanathan AN, et al. Consensus recommendations for radiation therapy contouring and treatment of vulvar carcinoma. Int J Radiat Oncol Biol Phys. 2016; 95: 1191-1200.
[16] Gupta S, Ahuja S, Kalwaniya DS, Shamsunder S, Solanki S. Vulval premalignant lesions: a review article. Obstet Gynecol Sci. 2024;67(2):169-185. doi:10.5468/ogs.23274
[17] Van Esch EM, Dam MC, Osse ME, Putter H, Trimbos BJ, Fleuren G, et al. Clinical characteristics associated with development of recurrence and progression in usual-type vulvar intraepithelial neoplasia. Int J Gynecol Cancer. 2013;23:1476–83. doi: 10.1097/IGC.0b013e3182a57fd6.