Pilot Phenotypic Mapping to Ambler Classes in Diabetic Urosepsis: Outcomes and Stewardship Insights
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
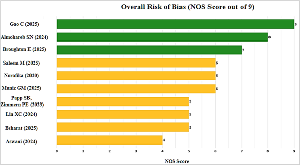
Background: Urosepsis occurs in uncontrolled diabetes mellitus (DM) with a high morbidity because of changing beta-lactam resistance, which may become a problem in the empiric treatment and clinical outcomes. Aim and Objective: The aim and objective of this study were to answer the research question: “How do phenotypic antibiotic resistance patterns in urosepsis among patients with uncontrolled diabetes mellitus map to the Ambler Classification of β-lactamases, and what are their associations with clinical outcomes such as acute kidney injury (AKI) and length of stay (LOS)?” Methods: A retrospective pilot cohort study was conducted at Karuna Medical College and Hospital that analyzed 17 urosepsis patients with uncontrolled DM. Available, clinical (HbA1c, serum creatinine/AKI, LOS, interventions, haemodialysis, mortality) and microbiological data were extracted. Descriptive and inferential tests were conducted. The phenotypic patterns were deduced on Ambler proxies, and polymerase chain reaction (PCR) was suggested to confirm them. Ten studies (2014-2025) were included in a systematic review and of them three in meta-analysis based on PubMed, Scopus, and Embase, random-effects modelling of Extended spectrum betalactamase (ESBL) prevalence. Results: AKI prevalence was 88.24%, mean LOS = 8.18 (SD 6.03), interventions = 11.76, and mortality was 0. The most common by prevalence was E. coli (47.06%); phenotypic inference suggested probably Class A in 52.94%. No significant associations were identified (all p>0.05). ESBL prevalence was 26.5% (95% CI -33.7 86.7) with high heterogeneity (I2=98.2%, p=0.001). Conclusion: Phenotypic patterns provide useful proxies of Ambler mapping to inform directed therapy, bypassing empiric shortcomings. PCR and AI combined studies should be carried out on a larger scale.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2026 Kiran D.R., S Veerakesari, Sarathlal S, Aleena Thomas Cheeran, Hariharan A, Pushpadasan P.R, Swathi N, Deena PM, Krishnendhu AM, Meenakshi C

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] J. C, R. K. A, S. R. Clinical and microbiological profile in intra-abdominal infection. Int Surg J [Internet]. 2019 Sep. 26 [cited 2026 Jan. 12];6(10):3608-13.
[2] CRISAN CM, PANDREA SL, TOMPA M, MOCAN T, PUIA A, MOCAN L. Escherichia coli infection, a negative prognostic factor on the evolution of patients with surgical diseases. Not Sci Biol [Internet]. 2022 Sep. 29 [cited 2026 Jan. 12];14(3):11344.
[3] Oh TH. Antimicrobial Therapy and Antimicrobial Stewardship in Urosepsis. Urogenit Tract Infect. 2023;18(1):15-19.
[4] Nocua-Báez LC, Cortés JA, Leal AL, Arias GF, Ovalle-Guerro MV, Saavedra-Rojas SY, Buitrago G, Escobar-Pérez JA, Castro-Cardozo B. [Antimicrobial susceptibility profile in urinary pathogens causing community-acquired infections in diabetic patients in Colombia]. Biomedica. 2017 Sep 1;37(3):353-360.
[5] Yunus R, Wijayati F, Askrening A, Rahayu DYS, Hasan FE, Trees T, Fusvita A. Diabetes Mellitus and Bacterial Infections: A Review of Main Infections in DM Patients. Public Health of Indonesia [Internet]. 2024 Mar. 21 [cited 2026 Jan. 12];10(1):73-97.
[6] Bassetti M, Ginocchio F, Mikulska M. New treatment options against gram-negative organisms. Crit Care. 2011;15(2):215.
[7] Tayeb SM, Alharbi JA, Alattas BB, Alotaibi DM, Althibaiti NM, Alharbi JF, Safir Aldeen AE, Alqurashi IR, Wali SM. Promising Future of Novel Beta-Lactam Antibiotics Against Bacterial Resistance. Drug Des Devel Ther. 2025 Oct 9;19:9185-9197.
[8] Bozcal E, Dagdeviren M. Toxicity of β-Lactam Antibiotics: Pathophysiology, Molecular Biology and Possible Recovery Strategies [Internet]. Poisoning - From Specific Toxic Agents to Novel Rapid and Simplified Techniques for Analysis. InTech; 2017.
[9] Almohareb SN, Aldairem A, Alsuhebany N, Alshaya OA, Aljatli D, Alnemer H, Almutairi K, Aljammaz N, Alowais SA. Effectiveness of oral antibiotics in managing extended-spectrum B-lactamase urinary tract infections: A retrospective analysis. SAGE Open Medicine. 2024.
[10] Gao C, Liu J, Wang D, Liu M, Qiu J. Risk factors and an optimized prediction model for urosepsis in diabetic patients with upper urinary tract stones. Scientific Reports. 2025 Mar 10;15(1):8183.
[11] Ibrahim SO, Elimam M, Taha SM, Yousif SM, Omer HM, Yousif M, Yassin S, Elnaiem A, Mohammed YA, Elhasan OA, Abakar AD. Urosepsis among Sudanese Patients: A Paradigm from Limited Resources Country. Advances in Microbiology. 2022 Mar 7;12(3):109-20.
[12] Chandra P, Anburaj SE, Vijayanarayana K, Vandana KE, Mukhopadhyay C, Acharya UD, Surulivelrajan M, Rajesh V. Outcome and attributable cost associated with bacterial resistant infections in a tertiary care hospital. Journal of Applied Pharmaceutical Science. 2023 Oct 4;13(10):132-40.
[13] Papp SB, Zimmern PE. Recurrent urinary tract infections and type 2 diabetes mellitus: a systematic review predominantly in women. Frontiers in Urology. 2023 Dec 12;3:1275334.
[14] Lin XC, Li CL, Zhang SY, Yang XF, Jiang M. The global and regional prevalence of hospital-acquired carbapenem-resistant Klebsiella pneumoniae infection: a systematic review and meta-analysis. In Open forum infectious diseases 2024 Feb (Vol. 11, No. 2, p. ofad649). US: Oxford University Press.
[15] Broughton E, Bektas M, Colosia A, Kuper K, Fernandez MM, Al-Taie A, Kotb R. A Systematic Literature Review of the Epidemiology of Complicated Urinary Tract Infection. Infectious Diseases and Therapy. 2025 Apr 24:1-25.
[16] Muñiz GM, Montesinos IL, León EP, Marinero AE, Montero M, Sorli L, Jorda XD, Horcajada JP. Prevalence, risk factors for and trends in faecal colonisation by extended-spectrum beta-lactamase-producing Enterobacterales (ESBL-PE) in the community in Spain: A cross-sectional study and meta-analysis. Enfermedades Infecciosas y Microbiología Clínica. 2025 Jun 1;43(6):323-30.
[17] Ahmad S, Hussain A, Khan MS, Shakireen N, Ali I. Diabetes mellitus and urinary tract infection: Causative uropathogens, their antibiotic susceptibility pattern and the effects of glycemic status. Pakistan Journal of Medical Sciences. 2020 Nov;36(7):1550.
[18] Ugur K, Bal IA, Tartar AS, Gozel N, Orhan B, Donder E, Ozercan AM. Ciprofloxacin is not a better choice in the patients with diabetes suffering urinary tract infection. Dicle Tıp Dergisi. 2019 Mar 1;46(1):65-72.
[19] Ajith A, Shamsundar BV, Kumari AB. A study on multidrug-resistant gram-negative bacilli from urinary samples in patients of a tertiary care centre. Int J Health Sci Res. 2025 Oct;15(10):176-184.
[20] Meghana G, Dsa ME, Yadav KNT. Development of antibiogram toolkit for enhancing empiric antibiotic selection in a tertiary care hospital. Int J Health Sci Res. 2024 Nov;14(11):383-390.
[21] Subramanian A, Bhat S, Mookkappan S, Anitha P, Kandasamy R, Kanungo R. Empiric antibiotic and in-vitro susceptibility of urosepsis pathogens: do they match? The outcome of a study from south India. The Journal of Infection in Developing Countries. 2021 Sep 30;15(09):1346-50.
[22] Ullah Z, Asghar J, Aziz N, Ullah A, Ashour AA, Felemban MF, Alqarni A, Shah SS, Quddoos A. Bacterial profiling and antibiotic resistance patterns in urinary tract infections: a microbiological analysis from Dera Isamil Khan, Pakistan. BMC Infectious Diseases. 2025 Sep 26;25(1):1151.
[23] Bsharat I, Sadaqa D, Shoeibat A, Rjoub H, Yaish M, Arafat H, Hindiyeh M, Sabateen A. Characterization of urosepsis in a tertiary hospital: 5-year retrospective study on prevalence and risk factors in Palestine. The Journal of Infection in Developing Countries. 2025 Oct 31;19(10):1479-86
[24] Aswani SM, Chandrashekar UK, Shivashankara KN, Pruthvi BC. Clinical profile of urinary tract infections in diabetics and non-diabetics. The Australasian medical journal. 2014 Jan 31;7(1):29.
[25] Ansari AS. Therapeutic options for the treatment of carbapenem-resistant Enterobacteriaceae infections: Hope in the times of hype and despair. Indian Journal of Critical Care Medicine: Peer-reviewed, Official Publication of Indian Society of Critical Care Medicine. 2021 Jul;25(7):752.
[26] Saleem M, Moursi SA, Altamimi TN, Alharbi MS, Alaskar AM, Hammam SA, Rakha E, Syed Muhammad OI, Almalaq HA, Alshammari MN, Syed Khaja AS. Prevalence and Molecular Characterization of Carbapenemase-Producing Multidrug-Resistant Bacteria in Diabetic Foot Ulcer Infections. Diagnostics. 2025 Jan 9;15(2):141.
[27] Arbianti N, Prihatiningsih S, Indriani DW, Indriati DW. A retrospective cross-sectional study of urinary tract infections and prevalence of antibiotic resistant pathogens in patients with diabetes mellitus from a public hospital in Surabaya, Indonesia. Germs. 2020 Sep 1;10(3):157.