Patterns of Anaesthesia in Orthopaedic and Trauma Surgery in Secondary Health Care Centre in South-Western Nigeria: A Retrospective Audit
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
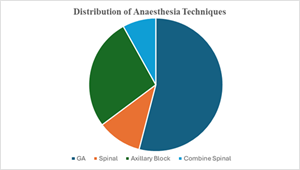
Background: Anaesthesia practice patterns in secondary care orthopaedic surgery in Nigeria remain understudied despite the critical role these facilities play in healthcare delivery. Understanding the relationship between anaesthetic technique selection, surgical duration, and postoperative outcomes is crucial for optimizing patient care and resource allocation in resource-limited settings. Objective: To analyse anaesthesia utilization patterns, examine correlations between anaesthetic techniques and surgical outcomes, and evaluate safety profiles in orthopaedic and trauma surgery at a Nigerian secondary healthcare centre. Methods: A retrospective descriptive study was conducted at Adeoyo State Hospital, Ibadan, over a 36-month period from January 2022 to December, 2024. Data from 62 consecutive orthopaedic surgical cases were analysed, including patient demographics, surgical procedures, anaesthesia types, surgical duration, hospital stay, and complications. Correlation analysis was performed to examine relationships between anaesthetic techniques and key outcomes using SPSS version 21. Results: Spinal anaesthesia was the predominant technique used in 45 cases (73.4%), followed by general anaesthesia in 10 cases (16.1%) and regional blocks in 5 cases (8.1%). Mean surgical duration was 3.2±1.4 hours across all cases, with no significant correlation between anaesthesia type and surgical duration (r=0.23, p=0.07). Mean hospital stay was 12.8±6.7 days, with anaesthesia technique showing no independent influence on length of stay (adjusted p=0.82). Blood transfusion was required in 26 cases (41.9%). No major anaesthesia-related complications were recorded, with an overall surgical complication rate of 6.5%. Conclusion: Spinal anaesthesia dominates orthopaedic anaesthesia practice in Nigerian secondary care settings while demonstrating versatility across surgical complexities and durations. The lack of correlation between neuraxial anaesthesia and prolonged surgical times or delayed recovery challenges conventional duration limitations, supporting the effectiveness of context-adapted anaesthetic protocols in resource-limited settings.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 O K Adebayo, O Koleosho-Ademua, J O Morhason-bello, A Allen-Taylor

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
O K Adebayo, Department of Anaesthesia, College of Medicine, University of Ibadan, Oyo State Nigeria.
Department of Anaesthesia, College of Medicine, University of Ibadan, Oyo State Nigeria.
O Koleosho-Ademua, Department of Anaesthesia, Ring Road State Hospital, Ibadan, Oyo state, Nigeria.
Department of Anaesthesia, Ring Road State Hospital, Ibadan, Oyo state, Nigeria.
J O Morhason-bello, Department of Orthopaedic and Trauma, University College Hospital, Ibadan, Oyo state, Nigeria.
Department of Orthopaedic and Trauma, University College Hospital, Ibadan, Oyo state, Nigeria.
A Allen-Taylor, Department of Orthopaedic and Trauma, Ring Road State Hospital, Ibadan, Oyo state, Nigeria.
Department of Orthopaedic and Trauma, Ring Road State Hospital, Ibadan, Oyo state, Nigeria.
[1] Memtsoudis SG, et al. Anesthesia-related risk factors for adverse outcomes after hip fracture surgery. Anesthesiology. 2020;133(4):719-732.
[2] Rashiq S, et al. Regional anesthesia vs general anesthesia for surgery. Cochrane Database Syst Rev. 2019;8:CD000521.
[3] Miller RD, et al. Miller's Anesthesia. 8th ed. Philadelphia: Elsevier Saunders; 2020.
[4] Adeyemo EA, et al. Anesthesia practice in Nigeria: A survey of current patterns. West Afr J Med. 2021;38(2):156-163.
[5] Olapade-Olaopa EO, et al. Surgical care in Nigeria: Challenges and opportunities. World J Surg. 2019;43(11):2737-2745.
[6] Karthikeyan P, et al. Comparison of spinal versus general anesthesia for lower limb orthopedic surgeries. Indian J Orthop. 2020;54(3):279-285.
[7] Horlocker TT, et al. Regional anesthesia in the patient receiving antithrombotic therapy. Reg Anesth Pain Med. 2018;43(3):263-309.
[8] Opperer M, et al. Does neuraxial anesthesia reduce intraoperative blood loss? Br J Anaesth. 2016;117(6):775-783.
[9] Nigerian Federal Ministry of Health. National Health Policy 2016: Promoting the Health of Nigerians to Accelerate Socio-economic Development. Abuja: FMOH; 2016.
[10] Basques BA, et al. General compared with spinal anesthesia for total hip arthroplasty. J Bone Joint Surg Am. 2015;97(6):455-461.
[11] Neuman MD, et al. Spinal anesthesia or general anesthesia for hip fracture surgery in older adults. N Engl J Med. 2021;385(22):2025-2035.
[12] Liu J, et al. Peripheral nerve blocks versus general anesthesia for total knee replacement in elderly patients on the postoperative quality of recovery. Clin Interv Aging. 2014;9:341-350.
[13] Johnson RL, et al. Neuraxial vs general anaesthesia for lower limb arthroplasty: a meta-analysis. Br J Anaesth. 2016;117(2):143-152.
[14] Pugely AJ, et al. A risk calculator for short-term morbidity and mortality after hip fracture surgery. J Orthop Trauma. 2014;28(2):63-69.
[15] Patorno E, et al. Comparative safety of anesthesia type for hip fracture surgery in adults. JAMA Intern Med. 2014;174(1):37-44.
[16] Afolabi BB, et al. Regional versus general anaesthesia for caesarean section. Cochrane Database Syst Rev. 2006;(4):CD004350.
[17] Macfarlane AJ, et al. Does regional anaesthesia improve outcome after total hip arthroplasty? A systematic review. Br J Anaesth. 2009;103(3):335-345.
[18] Idowu OK, et al. Spinal anaesthesia: patients and anaesthetists satisfaction. Afr Health Sci. 2011;11(3):297-300.
[19] Urwin SC, et al. General versus regional anaesthesia for hip fracture surgery: a meta-analysis of randomized trials. Br J Anaesth. 2000;84(4):450-455.
[20] O'Hara DA, et al. The benefits of regional anesthesia for lower extremity procedures. Anesth Analg. 1993;77(3):445-449.
[21] Fowler SJ, et al. Epidural analgesia compared with peripheral nerve blockade after major knee surgery: a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2008;100(2):154-164.
[22] Walker BJ, et al. Complications in pediatric regional anesthesia: an analysis from the Pediatric Regional Anesthesia Network. Anesthesiology. 2018;129(4):721-732.
[23] Beaupre LA, et al. Maximising functional recovery following hip fracture in frail seniors. Best Pract Res Clin Rheumatol. 2013;27(6):771-788.
[24] Griffiths R, et al. Perioperative care of the elderly 2014: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2014;69 Suppl 1:81-98.
[25] Rosencher N, et al. Orthopedic Surgery Transfusion Hemoglobin European Overview (OSTHEO) study: blood management in elective knee and hip arthroplasty in Europe. Transfusion. 2003;43(4):459-469.
[26] Omololu AB, et al. Complications of fracture treatment by traditional bone setters in southwest Nigeria. Fam Pract. 2002;19(6):625-629.
[27] Dada AA, et al. Complications of treatment of musculoskeletal injuries by bone setters. West Afr J Med. 2009;28(1):43-47.
[28] Onuminya JE, et al. Traditional bone setter's gangrene. Int Orthop. 1999;23(2):111-112.