HbA1c as a Determinant of Severity and Microbial Profile in Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
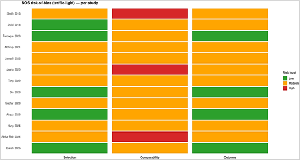
Background: Diabetic foot ulcers (DFUs) represent one of the most severe complications of diabetes mellitus and are caused by neuropathy, vascular insufficiency, and infection. Glycemic control as evidenced by glycated hemoglobin (HbA1c) has been proposed to affect ulcer severity and microbial colonization but the overall evidence has stayed fragmented. Objective: The entire objective of the systematic review and meta-analysis was to answer the query: "Is there a significant relation amongst levels of HbA1c, microbial spectrum, and severity in Wagner grade of diabetic foot ulcer patients?" Methods: A systematic review and meta-analysis was carried out in accordance with PRISMA guidance. Databases like PubMed, Embase, Scopus, Web of Science, and Cochrane Library were used to determine studies released from January 2016 to September 2025. Eligible studies were observational studies reporting HbA1c levels alongside Wagner grades and/or microbiological profiles. Data extraction was achieved using Microsoft Excel 2016 and then analysis in RStudio. A random-effects method was used to calculate pooled estimates on the odds of having severe diabetic foot ulcers (Wagner grade ≥3). Results: Thirteen studies in 1,976 patients were considered. There were four studies to be considered in meta-analysis. The overall percentage of patients with severe DFUs was 0.538 (95% CI: 0.430-0.645; p < 0.001). There was significant heterogeneity (I² = 73.7%, p = 0.034). Staphylococcus aureus and Pseudomonas aeruginosa were the predominant isolates and polymicrobial and resistant organisms were prevalent in advanced Wagner grades in the included studies. There was no visible publication bias by the funnel plot and Egger's regression test (p = 0.389). Conclusion: High HbA1c has strong correlation with greater severity of DFU (Wagner grade ≥3) and shifts in microbial spectrum towards resistant and polymicrobial infections. The findings highlight the need for strict glycemic control, early microbial profiling, and interdisciplinary management in the management of DFUs.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 S Pravin Dass, Meghna Mohan, V. Balaji Tulse Dass, Swathi N

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
S Pravin Dass, Faculty of Department of Urology, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Faculty of Department of Urology, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Meghna Mohan, Faculty of Department of General Medicine, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Faculty of Department of General Medicine, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
V. Balaji Tulse Dass, Faculty of Department of General Medicine, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Faculty of Department of General Medicine, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Swathi N, Data Analyst and Statistician, Department of Medical Research, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
Data Analyst and Statistician, Department of Medical Research, Karuna Medical College, Vilayodi, Chittur, Palakkad, Kerala, India.
[1] Edmonds M, Manu C, Vas P. The current burden of diabetic foot disease. J Clin Orthop Trauma. 2021 Feb 8;17:88-93. doi: 10.1016/j.jcot.2021.01.017.
[2] Fesseha BK, Abularrage CJ, Hines KF, Sherman R, Frost P, Langan S, Canner J, Likes KC, Hosseini SM, Jack G, Hicks CW, Yalamanchi S, Mathioudakis N. Association of Hemoglobin A1c and Wound Healing in Diabetic Foot Ulcers. Diabetes Care. 2018 Jul;41(7):1478-1485. doi: 10.2337/dc17-1683. Epub 2018 Apr 16.
[3] Monteiro-Soares M, Boyko EJ, Jeffcoate W, Mills JL, Russell D, Morbach S, Game F. Diabetic foot ulcer classifications: A critical review. Diabetes Metab Res Rev. 2020 Mar;36 Suppl 1:e3272.
[4] Mudrik-Zohar H, Carasso S, Gefen T, Zalmanovich A, Katzir M, Cohen Y, Paitan Y, Geva-Zatorsky N, Chowers M. Microbiome Characterization of Infected Diabetic Foot Ulcers in Association with Clinical Outcomes: Traditional Cultures Versus Molecular Sequencing Methods. Front Cell Infect Microbiol. 2022 Mar 24;12:836699.
[5] Smith K, Collier A, Townsend EM, O'Donnell LE, Bal AM, Butcher J, Mackay WG, Ramage G, Williams C. One step closer to understanding the role of bacteria in diabetic foot ulcers: characterising the microbiome of ulcers. BMC Microbiol. 2016 Mar 22;16:54.
[6] Ramanathan B, Duraisamy R, Venkatramanasami BTD, Abbas MK, Balamurugan A. Association of glycaemic status and outcomes in diabetic foot problems: a retrospective evidence from South India. J Basic Clin Physiol Pharmacol. 2021 Feb 22;33(2):155-162.
[7] Jneid J, Cassir N, Schuldiner S, Jourdan N, Sotto A, Lavigne JP, La Scola B. Exploring the Microbiota of Diabetic Foot Infections With Culturomics. Front Cell Infect Microbiol. 2018 Aug 14;8:282.
[8] Złoch M, Maślak E, Kupczyk W, Jackowski M, Pomastowski P, Buszewski B. Culturomics Approach to Identify Diabetic Foot Infection Bacteria. Int J Mol Sci. 2021 Sep 3;22(17):9574.
[9] Farooque U, Lohano AK, Hussain Rind S, Rind MS Sr, Karimi S, Jaan A, Yasmin F, Cheema O. Correlation of Hemoglobin A1c With Wagner Classification in Patients With Diabetic Foot. Cureus. 2020 Jul 15;12(7):e9199.
[10] Huang Y, Xie T, Cao Y, Wu M, Yu L, Lu S, Xu G, Hu J, Ruan H. Comparison of two classification systems in predicting the outcome of diabetic foot ulcers: the Wagner grade and the Saint Elian Wound score systems. Wound Repair Regen. 2015 May-Jun;23(3):379-85.
[11] Ning P, Liu Y, Kang J, Cao H, Zhang J. Comparison of healing effectiveness of different debridement approaches for diabetic foot ulcers: a network meta-analysis of randomized controlled trials. Front Public Health. 2023 Dec 11;11:1271706.
[12] R. AH, K. V. C, B. J, K. B. R, Pai G, M. A. B. Clinico-bacteriological study of diabetic foot ulcer and its management based on Wagner’s classification and HbA1c as an indicator for duration of antibiotic therapy in a tertiary hospital in Sullia. Int Surg J [Internet]. 2021 Jun. 28 [cited 2025 Sep. 13];8(7):2098-103.
[13] Raja JM, Maturana MA, Kayali S, Khouzam A, Efeovbokhan N. Diabetic foot ulcer: A comprehensive review of pathophysiology and management modalities. World J Clin Cases. 2023 Mar 16;11(8):1684-1693. doi: 10.12998/wjcc.v11.i8.1684.
[14] Jawzali JI, Muhammadamin HI, Othman AN, Ikram ZI. Association of glycated hemoglobin levels with severity of diabetic foot ulcer and bacterial profile [Internet]. J Diabetol. 2025 Jan 13 [cited 2025 Sep 13];16(1):43–9.
[15] Jnana A, Muthuraman V, Varghese VK, Chakrabarty S, Murali TS, Ramachandra L, Shenoy KR, Rodrigues GS, Prasad SS, Dendukuri D, Morschhauser A, Nestler J, Peter H, Bier FF, Satyamoorthy K. Microbial Community Distribution and Core Microbiome in Successive Wound Grades of Individuals with Diabetic Foot Ulcers. Appl Environ Microbiol. 2020 Mar 2;86(6):e02608-19.
[16] Shi ML, Quan XR, Tan LM, Zhang HL, Yang AQ. Identification and antibiotic susceptibility of microorganisms isolated from diabetic foot ulcers: A pathological aspect. Exp Ther Med. 2022 Dec 7;25(1):53.
[17] Baig MS, Banu A, Zehravi M, Rana R, Burle SS, Khan SL, Islam F, Siddiqui FA, Massoud EES, Rahman MH, Cavalu S. An Overview of Diabetic Foot Ulcers and Associated Problems with Special Emphasis on Treatments with Antimicrobials. Life (Basel). 2022 Jul 14;12(7):1054.
[18] Tong KPS, Green SJ, Ortiz J, Wu SC. Association between hemoglobin A1c, Vitamin C, and microbiome in diabetic foot ulcers and intact skin: A cross-sectional study. Health Sci Rep. 2022 Aug 3;5(5):e718.
[19] Ahmad S, Khan MSA, Shah MH, Khan A, Bano R, Qazi M. Microbial Profile and Antimicrobial Susceptibility Pattern in Diabetic Foot Ulcer Patients Attending a Tertiary Care Hospital. Cureus. 2022 Sep 30;14(9):e29770.
[20] Din N, Khan M, Danyal Khan B, Ghaffar T, Tabish Ikram M, Aamir Salman M, Khan Hadi N, Khan S. Association of Severity of Diabetic Foot Ulcer with Glycated Hemoglobin A1C Levels: Diabetic Foot Ulcer with Glycated HBA1C Levels. PJHS-Lahore [Internet]. 2023 Jan. 31 [cited 2025 Sep. 13];4(01):161-5.
[21] Lubis MIP, Marshal, Ali Syahputra M. Association of Glycosyllated Hemoglobin (Hba1c) Levels to the Severity of Diabetic Foot Ulcer in Type 2 Diabetes Mellitus Patients in RSUP. H. Adam Malik Medan. Sumat. Med. J. [Internet]. 2022Nov.10 [cited 2025Sep.13];5(1).
[22] Sachar RK, Rao H, Sharma PP, Aggarwal MP, Yadav S. Correlation of glycated haemoglobin status with the foot ulcer. Int Surg J [Internet]. 2023 Aug. 28 [cited 2025 Sep. 13];10(9):1461-70.
[23] Akyüz S, Bahçecioğlu Mutlu AB, Guven HE, Başak AM, Yilmaz KB. Elevated HbA1c level associated with disease severity and surgical extension in diabetic foot patients. Ulus Travma Acil Cerrahi Derg. 2023 Sep;29(9):1013-1018.
[24] Taki E, Jabalameli F, Mohajeri Tehrani MR, Feizabadi MM, Beigverdi R, Emaneini M. Microbial Profile and Antibiotic Susceptibility Pattern in Diabetic Patients with Mild, Moderate, and Severe Foot Infections in Tehran. Arch Razi Inst. 2022 Oct 31;77(5)
[25] Hung SY, Yeh YM, Chiu CH, Armstrong DG, Lin CW, Yang HM, Huang SY, Huang YY, Huang CH. Microbiome of limb-threatening diabetic foot ulcers indicates the association of fastidious Stenotrophomonas and major amputation. J Microbiol Immunol Infect. 2024 Feb;57(1):156-163.
[26] Pal B, Gupta SK. A study on the relation of the severity of diabetic foot ulcers with the type of bacterial flora isolated from the wounds. Int Surg J [Internet]. 2016 Dec. 13 [cited 2025 Sep. 13];3(1):189-94.
[27] Md. Abdur Rab, Md. Anisul Hossain, Shireen Begum, N. M Saifuddin Nizami, Lutfun Naher. Co-Relation
[28] Between Level of HbA1c and Depth of Diabetic Foot Ulcer. SAS J Surg, 2024 Oct 10(10): 1116-1123.
[29] Bahati R, Kitua D, Selestine L, Mwanga A, Urio M, Mchele G, Antanamsu D. Factors influencing the severity of diabetic foot ulcers: a cross-sectional study. BMC Endocr Disord. 2025 Mar 20;25(1):76. doi: 10.1186/s12902-024-01785-0.