Role of Procalcitonin after Paediatric Cardiac Surgery Under Cardiopulmonary Bypass and Its Correlation with Other Marker of Inflammation
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
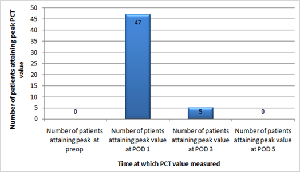
Objective: The effect of Cardiopulmonary bypass on serum Procalcitonin, and its correlation with other markers of inflammation in paediatric cardiac surgery patients. Design: A prospective observational study. Subjects/Patients: 52 paediatric patients requiring cardiac surgery under Cardiopulmonary bypass. Methods: Serum Procalcitonin, C-reactive protein and Total leukocyte count levels were measured preoperatively as baseline and then postoperatively on day 1, 3 and 5. Their kinetics and correlations were evaluated. Results: Peak levels of Procalcitonin showed a positive correlation with duration of Cardiopulmonary bypass time (rho=0.316, p= 0.02), aortic cross clamp time (rho=0.319, p=0.021), length of Intensive care unit stay (rho=0.418, p= 0.002). No correlation was observed between duration of Cardiopulmonary bypass or aortic cross clamp time and length of Intensive care stay with C-reactive protein or Total leukocyte count levels. Procalcitonin exhibits faster kinetics as compared to C-reactive protein and Total leukocyte count. Conclusions: Serial Procalcitonin measurements may be useful for identifying infections in the later post-operative period. However, Procalcitonin may not be considered an ideal biomarker for post-operative infections in paediatric cardiac surgery under Cardiopulmonary bypass, warranting further research.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dr. Sudhansoo Khanna, Prof. Rana Sandip Singh, Prof. Harkant Singh, Prof. Anand Kumar Mishra, Dr Virendra K Arya, Dr. Chetanya Singh Bhatti

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Zakkar M, Taylor K, Hornick PI. Immune System and Inflammatory Responses to Cardiopulmonary Bypass. In: Gravlee GP, Davis RF, Stammer AH, Ungerkeide RM, eds. Text book of Cardiopulmonary Bypass: Principles & Practice. 3rd ed. United States of America: Lippincot Williams & Wilkins; 2008: 332.
[2] Arkader R, Troster EJ, Lopes MR, Júnior RR, Carcillo JA, Leone C, et al. Procalcitonin does discriminate between sepsis and systemic inflammatory response syndrome. Arch Dis Child [Internet]. 2006 Feb [cited 2025 Mar 10];91(2):117-20. https://doi.org/10.1136/adc.2005.077446.
[3] Arkader R, Troster EJ, Abellan DM, Lopes MR, Júnior RR, Carcillo JA, et al. Procalcitonin and C-reactive protein kinetics in postoperative pediatric cardiac surgical patients. J Cardiothorac Vasc Anesth. 2004 Apr;18(2):160-5. https://doi.org/10.1053/j.jvca.2004.01.021.
[4] McMaster P, Park DY, Shann F, Cochrane A, Morris K, Gray J, et al. Procalcitonin versus C-reactive protein and immature-to-total neutrophil ratio as markers of infection after cardiopulmonary bypass in children. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2009 Mar;10(2):217-21. https://doi.org/10.1097/PCC.0b013e31819369f3.
[5] Sponholz C, Sakr Y, Reinhart K, Brunkhorst F. Diagnostic value and prognostic implications of serum procalcitonin after cardiac surgery: a systematic review of the literature. Crit Care Lond Engl. 2006;10(5): R145. https://doi.org/10.1186/cc5067.
[6] Celebi S, Koner O, Menda F, Balci H, Hatemi A, Korkut K, et al. Procalcitonin kinetics in pediatric patients with systemic inflammatory response after open heart surgery. Intensive Care Med. 2006 Jun;32(6):881-7. https://doi.org/10.1007/s00134-006-0180-z.
[7] Beghetti M, Rimensberger PC, Kalangos A, Habre W, Gervaix A. Kinetics of procalcitonin, interleukin 6 and C-reactive protein after cardiopulmonary-bypass in children. Cardiol Young. 2003 Apr;13(2):161-7. https://doi.org/10.1017/s1047951103000301.
[8] Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013 May;13(5):426-35. https://doi.org/10.1016/S1473-3099(12)70323-7.
[9] McWilliam S, Riordan A. How to use: C-reactive protein. Arch Dis Child Educ Pract Ed. 2010 Apr;95(2):55-8. https://doi.org/10.1136/adc.2009.174367.
[10] Macrina F, Tritapepe L, Pompei F, Sciangula A, Evangelista E, Toscano F, et al. Procalcitonin is useful whereas C-reactive protein is not, to predict complications following coronary artery bypass surgery. Perfusion. 2005 May;20(3):169-75. https://doi.org/10.1191/0267659105pf800oa.
[11] Loebe M, Locziewski S, Brunkhorst FM, Harke C, Hetzer R. Procalcitonin in patients undergoing cardiopulmonary bypass in open heart surgery-first results of the Procalcitonin in Heart Surgery study (ProHearts). Intensive Care Med. 2000 Mar;26 Suppl 2:S193-198. https://doi.org/10.1007/BF02900737.
[12] Prat C, Ricart P, Ruyra X, Domínguez J, Morillas J, Blanco S, et al. Serum concentrations of procalcitonin after cardiac surgery. J Card Surg. 2008;23(6):627-32. https://doi.org/10.1111/j.1540-8191.2008.00658.x.
[13] Nadziakiewicz P, Grochla M, Krauchuk A, Pióro A, Szyguła-Jurkiewicz B, Baca A, et al. Procalcitonin Kinetics After Heart Transplantation and as a Marker of Infection in Early Postoperative Course. Transplant Proc. 2020 Sep;52(7):2087-90. https://doi.org/10.1016/j.transproceed.2020.02.117.
[14] Nicolotti D, Grossi S, Palermo V, Pontone F, Maglietta G, Diodati F, et al. Procalcitonin for the diagnosis of postoperative bacterial infection after adult cardiac surgery: a systematic review and meta-analysis. Crit Care Lond Engl. 2024 Feb 7;28(1):44. https://doi.org/10.1186/s13054-024-04824-3.
[15] Allan CK, Newburger JW, McGrath E, Elder J, Psoinos C, Laussen PC, et al. The relationship between inflammatory activation and clinical outcome after infant cardiopulmonary bypass. Anesth Analg. 2010 Nov;111(5):1244-51. https://doi.org/10.1213/ANE.0b013e3181f333aa.
[16] Boehne M, Sasse M, Karch A, Dziuba F, Horke A, Kaussen T, et al. Systemic inflammatory response syndrome after pediatric congenital heart surgery: Incidence, risk factors, and clinical outcome. J Card Surg. 2017 Feb;32(2):116-25. https://doi.org/10.1111/jocs.12879.
[17] Haponiuk I, Jaworski R, Paczkowski K, Chojnicki M, Steffens M, Szofer-Sendrowska A, et al. Postoperative kinetics of common inflammatory biomarkers after congenital heart defect procedures with extracorporeal circulation in children. Kardiol Pol. 2018;76(6):968-73. https://doi.org/10.5603/KP.a2018.0038.
[18] Raja SG, Dreyfus GD. Modulation of systemic inflammatory response after cardiac surgery. Asian Cardiovasc Thorac Ann. 2005 Dec;13(4):382-95. https://doi.org/10.1177/021849230501300422.
[19] Jebali MA, Hausfater P, Abbes Z, Aouni Z, Riou B, Ferjani M. Assessment of the accuracy of procalcitonin to diagnose postoperative infection after cardiac surgery. Anesthesiology. 2007 Aug;107(2):232-8. https://doi.org/10.1097/01.anes.0000271871.07395.ad.
[20] Chakravarti SB, Reformina DA, Lee TM, Malhotra SP, Mosca RS, Bhatla P. Procalcitonin as a biomarker of bacterial infection in pediatric patients after congenital heart surgery. Ann Pediatr Cardiol [Internet]. 2016 [cited 2025 Mar 10];9(2):115-9. https://doi.org/10.4103/0974-2069.180665.
[21] Sharma P, Patel K, Baria K, Lakhia K, Malhotra A, Shah K, et al. Procalcitonin level for prediction of postoperative infection in cardiac surgery. Asian Cardiovasc Thorac Ann. 2016 May;24(4):344-9. https://doi.org/10.1177/0218492316640953.
[22] Li X, Wang X, Li S, Yan J, Li D. Diagnostic Value of Procalcitonin on Early Postoperative Infection After Pediatric Cardiac Surgery. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2017 May;18(5):420-8. https://doi.org/10.1097/PCC.0000000000001118.
[23] Carrasco-Castilla AI, Jiménez-González MDC, Cruz-García E, Gutiérrez-Tovar G, Cedillo-López AA, Rodríguez-López MER, et al. [Procalcitonin as sepsis predictor in cardiovascular surgery with cardiopulmonary bypass]. Rev Medica Inst Mex Seguro Soc. 2023 Nov 6;61(6):802-8. https://doi.org/10.5281/zenodo.10064366.
[24] Ghillani PP, Motté P, Troalen F, Jullienne A, Gardet P, Le Chevalier T, et al. Identification and measurement of calcitonin precursors in serum of patients with malignant diseases. Cancer Res. 1989 Dec 1;49(23):6845-51.
[25] D’Souza S, Guhadasan R, Jennings R, Siner S, Paulus S, Thorburn K, et al. Procalcitonin and Other Common Biomarkers Do Not Reliably Identify Patients at Risk for Bacterial Infection After Congenital Heart Surgery. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2019 Mar;20(3):243-51. https://doi.org/10.1097/PCC.0000000000001826.
[26] Renk H, Grosse D, Schober S, Schlensak C, Hofbeck M, Neunhoeffer F. Post-operative kinetics of C-reactive protein to distinguish between bacterial infection and systemic inflammation in infants after cardiopulmonary bypass surgery: the early and the late period. Cardiol Young. 2022 Jun;32(6):904-11. https://doi.org/10.1017/S1047951121003231.
[27] Boeken U, Feindt P, Micek M, Petzold T, Schulte HD, Gams E. Procalcitonin (PCT) in cardiac surgery: diagnostic value in systemic inflammatory response syndrome (SIRS), sepsis and after heart transplantation (HTX). Cardiovasc Surg Lond Engl. 2000 Dec;8(7):550-4. https://doi.org/10.1016/s0967-2109(00)00070-3.
[28] Aouifi A, Piriou V, Bastien O, Blanc P, Bouvier H, Evans R, et al. Usefulness of procalcitonin for diagnosis of infection in cardiac surgical patients. Crit Care Med. 2000 Sep;28(9):3171-6. https://doi.org/10.1097/00003246-200009000-00008.
[29] Skrak P, Kovacikova L, Kunovsky P. Procalcitonin, neopterin and C-reactive protein after pediatric cardiac surgery with cardiopulmonary bypass. Bratisl Lek Listy. 2007;108(12):501-5.
[30] Hammer S, Loeff M, Reichenspurner H, Daebritz S, Tiete A, Kozlik-Feldmann R, et al. Effect of cardiopulmonary bypass on myocardial function, damage and inflammation after cardiac surgery in newborns and children. Thorac Cardiovasc Surg. 2001 Dec;49(6):349-54. https://doi.org/10.1055/s-2001-19011.
[31] Séguéla PE, Joram N, Romefort B, Manteau C, Orsonneau JL, Branger B, et al. Procalcitonin as a marker of bacterial infection in children undergoing cardiac surgery with cardiopulmonary bypass. Cardiol Young. 2011 Aug;21(4):392-9. https://doi.org/10.1017/S104795111100014X.
[32] Nahum E, Schiller O, Livni G, Bitan S, Ashkenazi S, Dagan O. Procalcitonin level as an aid for the diagnosis of bacterial infections following pediatric cardiac surgery. J Crit Care. 2012 Apr;27(2):220.e11-16. https://doi.org/10.1016/j.jcrc.2011.07.076.
[33] Minami E, Ito S, Sugiura T, Fujita Y, Sasano H, Sobue K. Markedly elevated procalcitonin in early postoperative period in pediatric open heart surgery: a prospective cohort study. J Intensive Care. 2014;2(1):38. https://doi.org/10.1186/2052-0492-2-38.
[34] Farias JS, Villarreal EG, Dhargalkar J, Kleinhans A, Flores S, Loomba RS. C-reactive protein and procalcitonin after congenital heart surgery utilizing cardiopulmonary bypass: When should we be worried? J Card Surg. 2021 Nov;36(11):4301-7. https://doi.org/10.1111/jocs.15952.
[35] Casey WF, Hauser GJ, Hannallah RS, Midgley FM, Khan WN. Circulating endotoxin and tumor necrosis factor during pediatric cardiac surgery. Crit Care Med. 1992 Aug;20(8):1090-6. https://doi.org/10.1097/00003246-199208000-00004.
[36] Lequier LL, Nikaidoh H, Leonard SR, Bokovoy JL, White ML, Scannon PJ, et al. Preoperative and postoperative endotoxemia in children with congenital heart disease. Chest. 2000 Jun;117(6):1706-12. https://doi.org/10.1378/chest.117.6.1706.
[37] Klingele M, Bomberg H, Poppleton A, Minko P, Speer T, Schäfers HJ, et al. Elevated procalcitonin in patients after cardiac surgery: a hint to nonocclusive mesenteric ischemia. Ann Thorac Surg. 2015 Apr;99(4):1306-12. https://doi.org/10.1016/j.athoracsur.2014.10.064.
[38] Zant R, Stocker C, Schlapbach LJ, Mayfield S, Karl T, Schibler A. Procalcitonin in the Early Course Post Pediatric Cardiac Surgery. Pediatr Crit Care Med J Soc Crit Care Med World Fed Pediatr Intensive Crit Care Soc. 2016 Jul;17(7):624-9. https://doi.org/10.1097/PCC.0000000000000751.