Xanthogranulomatous Cholecystitis in a GBC Endemic Zone: Diagnostic Uncertainty Drives Unnecessary Extended Resection and Major Surgical Morbidity
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
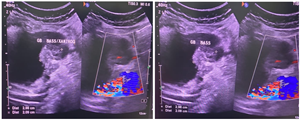
Background: Xanthogranulomatous Cholecystitis (XGC) is a benign inflammatory condition whose features often closely mimic Gallbladder Carcinoma (GBC). In GBC-endemic regions like Eastern India, this diagnostic uncertainty is intensified, frequently leading to unnecessary radical surgical intervention. This study aimed to characterize the clinical presentation, diagnostic limitations, and surgical burden of XGC in a high-risk cohort. Methods: This was a retrospective, single-center study of 48 patients with histopathologically confirmed pure XGC over a two-year period (Jan 2022–Dec 2023). Postoperative outcomes were rigorously assessed using the Clavien-Dindo classification. Results: The cohort showed a marked female predominance (62.5%) and mean age (53.8 years) consistent with local GBC demographics. Radiological non-specificity was profound: 91.7% of benign XGC cases exhibited mucosal gap/disruption, a feature conventionally associated with malignancy. This severe diagnostic uncertainty resulted in 37.5% of patients undergoing unnecessary extended resections, which translated to a high 20.8% major postoperative complication rate (Clavien-Dindo ≥IIIa). Conclusion: The high clinical and surgical burden of XGC demands an urgent institutional shift toward a definitive preoperative diagnosis, necessitating immediate review of imaging and frozen section standards. The essential next step is a prospective, multi-center study to develop and validate a Machine Learning (ML)-based predictive nomogram to ensure the diagnostic certainty required for safe, conservative XGC management.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2026 Dr. Pushpanjali Behera, Dr. Anup Kumar Pramanik, Dr. Bagmi Mishra, Dr. Sashibhusan Dash

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Makimoto S, Takami T, Hatano K, Kataoka N, Yamaguchi T, Tomita M, Shono Y. Xanthogranulomatous cholecystitis: a review of 31 patients. Surg Endosc. 2021 Jul;35(7):3874-3880. doi: 10.1007/s00464-020-07828-6.
[2] Feng L, You Z, Gou J, Liao E, Chen L. Xanthogranulomatous cholecystitis: experience in 100 cases. Ann Transl Med. 2020 Sep;8(17):1089. doi: 10.21037/atm-20-5836.
[3] Akkurt G, Birben B, Çoban S, Akgül Ö, Kulaçoğlu S, Doğanay M. Xanthogranulomatous Cholecystitis and Gallbladder Cancer: Two Diseases with Difficult Differential Diagnoses. Turk J Gastroenterol. 2021 Aug;32(8):694-701. doi: 10.5152/tjg.2021.201006.
[4] Yang T, Zhang BH, Zhang J, Zhang YJ, Jiang XQ, Wu MC. Surgical treatment of xanthogranulomatous cholecystitis: experience in 33 cases. Hepatobiliary Pancreat Dis Int. 2007 Oct;6(5):504-8.
[5] Suzuki H, Wada S, Araki K, Kubo N, Watanabe A, Tsukagoshi M, Kuwano H. Xanthogranulomatous cholecystitis: Difficulty in differentiating from gallbladder cancer. World J Gastroenterol. 2015 Sep 21;21(35):10166-73. doi: 10.3748/wjg.v21.i35.10166.
[6] Dutta U, Bush N, Kalsi D, Popli P, Kapoor VK. Epidemiology of gallbladder cancer in India. Chin Clin Oncol. 2019 Aug;8(4):33. doi: 10.21037/cco.2019.08.03.
[7] Hale MD, Roberts KJ, Hodson J, Scott N, Sheridan M, Toogood GJ. Xanthogranulomatous cholecystitis: a European and global perspective. HPB (Oxford). 2014 May;16(5):448-58. doi: 10.1111/hpb.12152.
[8] Khan I, Panda N, Banerjee M, Das R. Epidemiological factors in gall bladder cancer in eastern India-a single centre study. Indian J Surg Oncol. 2013 Mar;4(1):67-72. doi: 10.1007/s13193-012-0203-x.
[9] Deng YL, Cheng NS, Zhang SJ, Ma WJ, Shrestha A, Li FY, Xu FL, Zhao LS. Xanthogranulomatous cholecystitis mimicking gallbladder carcinoma: An analysis of 42 cases. World J Gastroenterol 2015; 21(44): 12653-12659.doi: 10.3748/wjg.v21.i44.12653]
[10] Chang BJ, Kim SH, Park HY, Lim SW, Kim J, Lee KH, Lee KT, Rhee JC, Lim JH, Lee JK. Distinguishing xanthogranulomatous cholecystitis from the wall-thickening type of early-stage gallbladder cancer. Gut Liver. 2010 Dec;4(4):518-23. doi: 10.5009/gnl.2010.4.4.518.
[11] Suzuki H. Specific radiological findings, if present, can offer high accuracy for the differentiation of Xanthogranulomatous cholecystitis and gallbladder cancer. Ann Transl Med. 2020 Jun;8(11):662. doi: 10.21037/atm.2020.03.193.
[12] Pandey A, Kumar D, Masood S, Chauhan S, Kumar S. Is Final Histopathological Examination the Only Diagnostic Criteria for Xanthogranulomatous Cholecystitis? Niger J Surg. 2019 Jul-Dec;25(2):177-182. doi: 10.4103/njs.NJS_1_19.
[13] Yüksel E, Dinçer B, Ömeroğlu S. Factors affecting the risk of conversion from laparoscopy to open surgery in xanthogranulomatous cholecystitis: a retrospective cohort study. BMC Surg. 2025 Sep 29;25(1):416. doi: 10.1186/s12893-025-03097-z.
[14] Noji T, Takeuchi S, Wada M, Tanaka K, Matsui A, Nakanishi Y, Asano T, Nakamura T, Kawamoto Y, Hirano S. Short- and Long-term Surgical Results of Extended Surgery for Widespread Gallbladder Carcinoma. In Vivo. 2025 Mar-Apr;39(2):1022-1032. doi: 10.21873/invivo.13907.