A Prospective Study of Abdominal Wound Dehiscence in a Tertiary Care Hospital
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
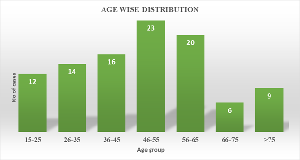
Background: Abdominal wound dehiscence is defined as the postoperative separation of layers of a wound, with or without eventration. AWD is one of the most feared postoperative complications for surgeons and is of great concern because of the risk of burst abdomen, the need for immediate intervention, and the possibility of repeat dehiscence, surgical site infection, and mortality. Objective: To estimate the burden of cases of abdominal wound dehiscence in elective and emergency operations, and to identify the aetiology and risk factors responsible for it. Design: A Prospective study was conducted, where the data was collected over a period of one year, from 1st June 2023 to 31st May 2024, in patients attending Government Medical College Jammu, who developed wound dehiscence after undergoing laparotomy for management of abdominal diseases. Subjects/Patients: The patients who had undergone laparotomy and developed wound dehiscence. Methods: A prospective observational study was carried out over a period of one year, from June 1, 2023, to May 31, 2024, in patients attending Government Medical College Jammu who developed wound dehiscence after laparotomy. Inclusion criteria included Patients of age > 14 years and of either sex who underwent either emergency or elective abdominal operations and developed wound dehiscence. Exclusion criteria: All patients with incisional hernia and patients with wound dehiscence on sites other than the abdomen. Results: Laparotomy wound dehiscence was more common in 46-55 years age group with a male-to-female ratio of 2.3:1 the incidence was higher in Emergency surgeries and those performed during night. Dirty wounds and Midline laparotomy had higher risk. Layered closure, of the abdomen, showed a higher rate of dehiscence compared to mass closure. Incidence was higher in BMI greater than 25, with haemoglobin levels below 10 g%, Albumin <3.5gm/dl, Proteins <6gm/dl. Average hospital stay was 22 days and mortality rate in our study was 8%. Conclusion: Keeping in view the morbidity, increased hospital stays, medical expenses, time lost to work, disabilities with future incisional hernia formation and mortality associated with abdominal wall dehiscence, the risk factors should be identified, preoperative optimisation should be done, corrective measures should be taken while closing abdomen and standard protocols should be followed to prevent wound dehiscence.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Vikrant Singh, Sanjay Sharma, Raja Langer, Priya Manhas, Vanita Gupta, Riya Singh Chandail

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Vikrant Singh, Associate Professor, Department of Surgical Gastroenterology, Government Medical College Jammu, India.
Associate Professor, Department of Surgical Gastroenterology, Government Medical College Jammu, India.
Sanjay Sharma, Associate Professor, Department of General Surgery, Government Medical College Jammu, India.
Associate Professor, Department of General Surgery, Government Medical College Jammu, India.
Raja Langer, Assistant Professor, Department of General Surgery, Government Medical College Jammu, India.
Assistant Professor, Department of General Surgery, Government Medical College Jammu, India.
Priya Manhas, Senior resident, Department of General Surgery, Government Medical College Jammu, India.
Senior resident, Department of General Surgery, Government Medical College Jammu, India.
Vanita Gupta, Professor, Department of Anatomy, SMVDIME, Kakryal, Katra, Jammu, India.
Professor, Department of Anatomy, SMVDIME, Kakryal, Katra, Jammu, India.
Riya Singh Chandail, MBBS Student ASCOMS Sidhra, Jammu, India.
MBBS Student ASCOMS Sidhra, Jammu, India.
[1] Carlson MA. Acute wound failure. Surg Clin North Am. 1997; 77:607–636. doi:10.1016/S0039-6109(05)70571-5.
[2] Savage A, Lamont M. Oxford textbook of surgery. Alison Langton; 2000. Wound dehiscence, incisional hernia, and parastomal hernia; p. 1883.
[3] Wong SY, Kingsnorth AN. Abdominal wound dehiscence and incisional hernia surgery. Surg (Oxford). 2002;20(5):100–3.
[4] Riou JP, Cohen JR, Johnson H Jr. Factors influencing wound dehiscence. Am J Surg. 1992; 163:324–30.
[5] Webster C, Neumayer L, Smout R, et al. Prognostic models of abdominal wound dehiscence after laparotomy. J Surg Res. 2003; 109:130–7.
[6] Bhangu A, Singh P, Lundy J, Bowley DM. Systematic review and meta-analysis of randomized clinical trials comparing primary vs. delayed primary skin closure in contaminated and dirty abdominal incisions. JAMA Surg. 2013; 148:779–86.
[7] Pandey S, Singh M, Singh K, Sandhu S. A prospective randomized study comparing non-absorbable polypropylene and delayed absorbable polyglactin 910 suture material in mass closure of vertical laparotomy wounds. Indian J Surg. 2013; 75:10–4.
[8] Tolstrup MB, Watt SK, Gögenur I. Reduced Rate of Dehiscence After Implementation of a Standardized Fascial Closure Technique in Patients Undergoing Emergency Laparotomy. Ann Surg. 2017
[9] Dugar D, Goel S. Intra-abdominal pressure measurement as a predictor of postoperative wound complications in patients undergoing emergency laparotomy: A prospective observational study. Cureus. 2024 Feb 25;16(2): e54860.
[10] Waqar SH, Malik ZI, Razzaq A, Abdullah MT. Frequency and risk factors for wound dehiscence/burst abdomen in midline laparotomies. J Ayub Med Coll Abbottabad. 2005;17:70–73. (Regional journal — DOI not found).
[11] Spiliotis J, Tsiveriotis K, Datsis AD, et al. Wound dehiscence: is still a problem in the 21th century: a retrospective study. World J Emerg Surg. 2009;4:12. doi:10.1186/1749-7922-4-12.
[12] Penninckx FM, Poelmans SV, Kerremans RP, et al. Abdominal wound dehiscence in gastroenterological surgery. Ann Surg. 1979;189:345–352. doi:10.1097/00000658-197903000-00016.
[13] Van Ramshorst GH et al, Van Ramshorst GH, Nieuwenhuizen J, Hop WC, et al. Abdominal wound dehiscence in adults: development and validation of a risk model. World J Surg. 2010;34:20–27. doi:10.1007/s00268-009-0277-y.
[14] Afzal S et al., Afzal S, Bashir MM. Determinants of wound dehiscence in abdominal surgery in public sector hospital. Ann King Edward Med Univ. 2008;14:110–115. (PDF on journal site — DOI not available).
[15] Gislason H, Grønbech JE, Søreide O. Burst abdomen and incisional hernia after major gastrointestinal operations — comparison of three closure techniques. Eur J Surg. 1995;161:349–354. (PubMed indexed — DOI not listed).
[16] Niggebrugge AH, Hansen BE, Trimbos JB, et al. Mechanical factors influencing the incidence of burst abdomen. Eur J Surg. 1995;161:655–61.
[17] Pavlidis TE, Galatianos IN, Papaziogas BT, et al. Complete dehiscence of the abdominal wound and incriminating factors. Eur J Surg. 2001;167:351–354. doi:10.1080/110241501750215221.
[18] Webster C, Neumayer L, Smout R, et al. Prognostic models of abdominal wound dehiscence after laparotomy. J Surg Res. 2003;109:130–137. doi:10.1016/S0022-4804(02)00097-5.
[19] Swaroop M, Williams M, Greene WR, et al. Multiple laparotomies are a predictor of fascial dehiscence in the setting of severe trauma. Am Surg. 2005;71:402–5.
[20] Parmar G, Gohil A, Hathila V. Burst abdomen: a grave postoperative complication. Internet J Surg. 2008;20:1–8. (Internet Journal — DOI not listed).
[21] Lozada Hernández EE et al., (2013) Abdominal wound dehiscence and incisional hernia prevention in midline laparotomy: a systematic review and network meta-analysis. Langenbecks Arch Surg. 2023 Jul 7;408(1):268. doi: 10.1007/s00423-023-02954-w. PMID: 37418033.
[22] Ceydeli A, Rucinski J, Wise L. Finding the best abdominal closure: an evidence-based review of the literature. Curr Surg. 2005;62:220–225. doi:10.1016/j.cursur.2004.08.014.
[23] Cengiz Y, Gislason H, Svanes K, Israelsson LA. Mass closure technique: an experimental study on separation of wound edge. Eur J Surg. 2001;167:60–63. doi:10.1080/110241501750069846
[24] Chiang RA, Chen SL, Tsai YC. Delayed primary closure versus primary closure for wound management in perforated appendicitis: A prospective randomized controlled trial. J Chin Med Assoc. 2012;75:156–9.
[25] Duttaroy DD, Jitendra J, Duttaroy B, Bansal U, Dhameja P, Patel G, et al. Management strategy for dirty abdominal incisions: Primary or delayed primary closure?. A randomized trial. Surg Infect (Larchmt). 2009;10:129–36.
[26] Chatwiriyacharoen W. Surgical wound infection post-surgery in perforated appendicitis in children. J Med Assoc Thai. 2002;85:572–6.
[27] Campuzano TIJ, López JDS, Malagón L et al., Risk factors and management of wound dehiscence in abdominal surgery. Int J Med Sci Clin Res Stud. 2023;3(11):10–16.
[28] Jaiswal NK et al.,(29) Jaiswal NK, Shekhar S. Study of burst abdomen: its causes and management. Int Surg J. 2018;5:1035–1040. doi:10.18203/2349-2902.isj20180826.
[29] Kapoor K, Hassan M. A clinical study of abdominal wound dehiscence with emphasis on surgical management in Bangalore Medical College and Research Institute, Karnataka, India. Int Surg J. 2017;4:134–140. doi:10.18203/2349-2902.ISJ20164078.
[30] Mahey R et al., (Mahey R, Ghetla S, Rajpurohit J, Desai D, Suryawanshi S. A prospective study of risk factors for abdominal wound dehiscence. Int Surg J. 2016;4:24–8.
[31] Choudhury A et al., (33 Choudhury A, Deka RK, Gogoi B, Kumar N. A clinical study of abdominal wound dehiscence including its causes and management. J Evol Med Dent Sci. 2017;6:1519–23.