A Comparative Evaluation of Hyperbaric Ropivacaine Versus Hyperbaric Bupivacaine for Lower Limb Surgeries
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
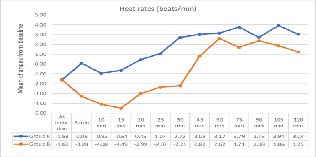
Background: Anesthesiologists frequently utilize various local anesthetics for intrathecal administration, including isobaric or hyperbaric formulations of ropivacaine, levobupivacaine, and bupivacaine solutions. Among these, hyperbaric local anesthetics like ropivacaine, levobupivacaine, and bupivacaine solutions are particularly prevalent. Aim of this study to compare the clinical efficacy and safety of hyperbaric 0.75% ropivacaine and hyperbaric 0.5% bupivacaine under spinal anaesthesia for lower limb surgeries, focusing on sensory and motor block characteristics. Methods: A randomized double-blind, prospective study, total 130 patients aged 18-50 undergoing lower limb surgeries. The study excluded patients with unwillingness, psychiatric diseases, emergency surgeries, drug abuse history, medical complications, coagulation disorders, local infections, spinal deformities, heart block or dysrrhythmia, sensory block not achieved till T10 level, and motor block less than 3(BS-3). Patients in the study were categorized into two groups: one receiving 0.75% ropivacaine and the other receiving 0.5% bupivacaine for spinal anaesthesia. The main objective was to investigate the effects of ropivacaine on spinal anaesthesia outcomes. Results: Total of 130 patients were analyzed, comparing the demographics and clinical parameters between two groups, R and B. The mean age of participants was 40.36±9.76 years, with average weight and height at 66.94±15.53 kg and 164.22±14.79 cm, respectively. Both groups had similar mean surgical durations, 120.74 minutes for group R and 121.01 minutes for group B. While group B exhibited shorter sensory and motor blockade durations, group R showed longer times. Bromage scores were found to be comparable between the two groups. Conclusion: The study compared ropivacaine and bupivacaine in spinal anesthesia duration, finding no significant difference. Bupivacaine had longer sensory blocking and motor blockage time, while ropivacaine had superior hemodynamic stability.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dr Satyendra Singh Yadav, Dr Pallavee Priyadarshini

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Dr Pallavee Priyadarshini, Assistant Professor, Department of Anaesthesiology, GSVM Medical College, Kanpur-208002, Uttar Pradesh, India.
Assistant Professor, Department of Anaesthesiology, GSVM Medical College, Kanpur-208002, Uttar Pradesh, India.
[1] J., A. Spinal anaesthesia. Nature 1909;82: 99.
[2] Uppal V, Retter S, Shanthanna H, Prabhakar C, McKeen DM. Hyperbaric versus isobaric bupivacaine for spinal anesthesia: systematic review and meta-analysis for adult patients undergoing noncesarean delivery surgery. Anesthesia & Analgesia. 2017 Nov 1;125(5):1627-37.
[3] Foster RH, Markham A. Levobupivacaine: A review of its pharmacology and use as a local anaesthetic. Drugs. 2000;59(3):551–579.
[4] del-Rio-Vellosillo M, Garcia-Medina JJ, Abengochea-Cotaina A, Pinazo-Duran MD, Barbera-Alacreu M. Spinal anesthesia for knee arthroscopy using isobaric bupivacaine and levobupivacaine: anesthetic and neuroophthalmological assessment. BioMed research international. 2014 Jan 1;2014.
[5] Broadbent CR, Maxwell WB, Ferrie R, Wilson DJ, Gawne‐Cain M, Russell R. Ability of anaesthetists to identify a marked lumbar interspace. Anaesthesia. 2000 Nov;55(11):1122-6.
[6] Albright GA. Cardiac arrest following regional anesthesia with etidocaine or bupivacaine. The Journal of the American Society of Anesthesiologists. 1979 Oct 1;51(4):285-7.
[7] Åkerman B, Hellberg IB, Trossvik C. Primary evaluation of the local anaesthetic properties of the amino amide agent ropivacaine (LEA 103). Acta anaesthesiologica scandinavica. 1988 Oct;32(7):571-8.
[8] McClure JH. Ropivacaine. British journal of anaesthesia. 1996 Feb 1;76(2):300-7.
[9] McClellan KJ, Faulds D. Ropivacaine: an update of its use in regional anaesthesia. Drugs. 2000 Nov; 60:1065-93.
[10] McDonald SB, Liu SS, Kopacz DJ, Stephenson CA. Hyperbaric spinal ropivacaine: a comparison to bupivacaine in volunteers. The Journal of the American Society of Anesthesiologists. 1999 Apr 1;90(4):971-7.
[11] Malinovsky JM, Charles F, Kick O, Lepage JY, Malinge M, Cozian A, Bouchot O, Pinaud M. Intrathecal anesthesia: ropivacaine versus bupivacaine. Anesthesia & analgesia. 2000 Dec 1;91(6):1457-60.
[12] Reiz S, Häggmark S, Johansson G, Nath S. Cardiotoxicity of ropivacaine–a new amide local anaesthetic agent. Acta Anaesthesiologica Scandinavica. 1989 Feb;33(2):93-8.
[13] Scott DB, Lee A, Fagan D, Bowler GM, Bloomfield P, Lundh R. Acute toxicity of ropivacaine compared with that of bupivacaine. Anesthesia & Analgesia. 1989 Nov 1;69(5):563-9.
[14] Nightingale PJ, Marstrand T. Subarachnoid anaesthesia with bupivacaine for orthopaedic procedures in the elderly. BJA: British Journal of Anaesthesia. 1981 Apr 1;53(4):369-71.
[15] Sule AZ, Isamade ES, Ekwempu CC. Spinal anaesthesia in lower abdominal and limb surgery: A review of 200 cases. Nigerian Journal of surgical research. 2005;7(1):226-30.
[16] Brull R, Macfarlane AJ, Chan VW. Spinal, epidural, and caudal anesthesia. Miller's anesthesia. 2015; 8:1684-716.
[17] McNamee DA, McClelland AM, Scott S, Milligan KR, Westman L, Gustafsson U, et al. Spinal anaesthesia: Comparison of plain ropivacaine 5 mg ml(-1) with bupivacaine 5 mg ml(-1) for major orthopaedic surgery. Br J Anaesth. 2002; 89:702–6.
[18] Mahajan HM, Patel SJ. To compare the efficacy of intrathecal 0.75% heavy ropivacaine and 0.5% heavy bupivacaine for lower abdominal and lower limb surgery. Asian Journal of Medical Sciences. 2023 Sep 1;14(9).
[19] Dar FA, Mushtaq MB, Khan UM. Hyperbaric spinal ropivacaine in lower limb and hip surgery: A comparison with hyperbaric bupivacaine. Journal of Anaesthesiology Clinical Pharmacology. 2015 Oct 1;31(4):466-70.
[20] Adhikari P, Vyas V, Naseem S, Shelke U. Comparative efficacy and safety of intrathecal ropivacaine versus intrathecal bupivacaine in patients undergoing lower abdominal surgical procedures. Indian Journal of Pain. 2020 Jan 1;34(1):43-6.
[21] Olapour A, Akhondzadeh R, Rashidi M, Gousheh M, Homayoon R. Comparing the effect of bupivacaine and ropivacaine in cesarean delivery with spinal anesthesia. Anesthesiology and pain medicine. 2020 Feb;10(1).
[22] Chari VR, Goyal A, Sengar P, Wani N. Comparison between intrathecal isobaric ropivacaine 0.75% with hyperbaric bupivacaine 0.5%: A double blind randomized controlled study. Anaesth Pain & Intensive Care. 2013;17(3):261-6.
[23] Purohit S, Badami R, Kavi C. Comparison of intrathecal 0.5% hyperbaric bupivacaine with 0.5% hyperbaric ropivacaine in lower limb and lower abdominal surgery. J Med Sci Clin Res. 2017;5(8):26995-7002.
[24] Kulkarni KR, Deshpande S, Namazi I, Singh SK, Kondilya K. A comparative evaluation of hyperbaric ropivacaine versus hyperbaric bupivacaine for elective surgery under spinal anesthesia. Journal of Anaesthesiology Clinical Pharmacology. 2014 Apr 1;30(2):238-42.
[25] Nisarga R, Nandini RT, Ramesh R. A comparative study of plain and hyperbaric solutions of 0.75% ropivacaine in spinal anaesthesia in elective lower abdominal and lower limb surgeries. IJMA. 2021;4(2):40-3.
[26] Erturk E, Tutuncu C, Eroglu A, Gokben M. Clinical comparison of 12 mg ropivacaine and 8 mg bupivacaine, both with 20 µg fentanyl, in spinal anaesthesia for major orthopaedic surgery in geriatric patients. Medical Principles and Practice. 2010 Feb 4;19(2):142-7.
[27] Bigat Z, Boztug N, Karsli B, Cete N, Ertok E. Comparison of hyperbaric ropivacaine and hyperbaric bupivacaine in unilateral spinal anaesthesia. Clinical drug investigation. 2006 Jan; 26:35-41.
[28] Beaulieu P, Babin D, Hemmerling T. The pharmacodynamics of ropivacaine and bupivacaine in combined sciatic and femoral nerve blocks for total knee arthroplasty. Anesthesia & Analgesia. 2006 Sep 1;103(3):768-74.
[29] Al-Abdulhadi O, Biehl D, Ong B, Boker A. Hyperbaric spinal for elective cesarean section. MEJ Anesth. 2007;19(2).
[30] Kharat, P. A., & Deopujari, R. C. A comparison of intrathecal 0.5% hyperbaric ropivacaine with 0.5% hyperbaric bupivacaine for elective surgery: a prospective, randomized, double-blind, controlled study. International Journal of Research in Medical Sciences, 2021;9(2):471-478.
[31] Kalbande JV, Kukanti C, Karim HM, Sandeep G, Dey S. The Efficacy and Safety of Spinal Anesthesia with Hyperbaric Ropivacaine 0.75% and Bupivacaine 0.5% in Patients Undergoing Infra-Umbilical Surgeries: A Randomized, Double-Blind Study. Cureus. 2024 Mar;16(3).