C-Reactive Protein Trends and Prediction of Anastomotic Leak in Esophageal Atresia
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
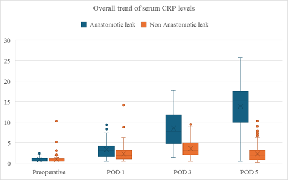
Objective: C-reactive protein (CRP), an acute phase reactant, has been proposed as an early biomarker for anastomotic leak in such patients. Design: Retrospective, single center, observational study. Patients: A cohort of 202 postoperative patients, with serum CRP levels measured on postoperative day (POD) 1, 3, and 5. Methods: Patients were stratified according to the presence of anastomotic leak (n=41) versus no leak (n=161). Group differences were assessed, and analysis was performed to evaluate diagnostic accuracy and determine optimal cutoff values. Result: Mean CRP levels were significantly higher in patients with anastomotic leaks compared to those without, with differences becoming most pronounced after POD 3. Statistical testing confirmed significant differences at POD 1 (p<0.01), POD 3 (p<1×10⁻⁹), and POD 5 (p<1×10⁻¹⁵). ROC analysis demonstrated increasing discriminatory power across time points: AUC 0.64 (POD1), 0.85 (POD3), and 0.94 (POD5). Optimal CRP cutoffs were identified as 2.7 mg/dl (POD1, sensitivity 61%, specificity 70%), 6.7 mg/dl (POD3, sensitivity 68%, specificity 89%), and 7.5 mg/dl (POD5, sensitivity 93%, specificity 98%). Conclusion: Elevated postoperative CRP levels, particularly on POD3 and POD5, are strongly associated with the occurrence of anastomotic leak. A CRP threshold of approximately 7 mg/dl on POD3 may serve as an early warning indicator, while levels above 7.5 mg/dl on POD5 provide excellent diagnostic accuracy. Routine CRP monitoring can therefore facilitate earlier detection and timely intervention in patients with anastomotic complications.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dr. Ashish Paliwal, Dr. Vinita Chaturvedi, Dr. Neeraj Tuteja, Dr. Ajay Jhalani, Dr. Aditya J Baindur, Dr. Ashok Chopra, Dr. Pankaj Goyal, Dr. Atul Kumar Khare

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Dr. Ashish Paliwal, MCH Resident, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
MCH Resident, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
Dr. Vinita Chaturvedi, Senior Professor and Head of Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
Senior Professor and Head of Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
Dr. Neeraj Tuteja, Associate Professor, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
Associate Professor, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
Dr. Ajay Jhalani, Assistant Professor, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
Assistant Professor, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
Dr. Aditya J Baindur, MCH Resident, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
MCH Resident, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
Dr. Ashok Chopra, MCH Resident, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
MCH Resident, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
Dr. Pankaj Goyal, MCH Resident, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
MCH Resident, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
Dr. Atul Kumar Khare, MCH Resident, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
MCH Resident, Department of Pediatrics Surgery, Sawai Man Singh, Medical College and Hospital, Jaipur, Rajasthan.
[1] Nassar N, Leoncini E, Amar E, Arteaga-Vázquez J, Bakker MK, Bower C, et al. Prevalence of esophageal atresia among 18 international birth defects surveillance programs. Birt Defects Res A Clin Mol Teratol. 2012 Nov;94(11):893-9.
[2] Van Lennep M, Singendonk MMJ, Dall’Oglio L, Gottrand F, Krishnan U, Terheggen-Lagro SWJ, et al. Oesophageal atresia. Nat Rev Dis Primer. 2019 Apr 18;5(1):26.
[3] Rothenberg S. Thoracoscopic repair of esophageal atresia and tracheo-esophageal fistula in neonates: the current state of the art. Pediatr Surg Int. 2014 Oct 1;30(10):979-85.
[4] Lal DR, Gadepalli SK, Downard CD, Ostlie DJ, Minneci PC, Swedler RM, et al. Perioperative management and outcomes of esophageal atresia and tracheoesophageal fistula. J Pediatr Surg. 2017 Aug;52(8):1245-51.
[5] Serhal L, Gottrand F, Sfeir R, Guimber D, Devos P, Bonnevalle M, et al. Anastomotic stricture after surgical repair of esophageal atresia: frequency, risk factors, and efficacy of esophageal bougie dilatations. J Pediatr Surg. 2010 July;45(7):1459-62.
[6] Okamoto T, Takamizawa S, Arai H, Bitoh Y, Nakao M, Yokoi A, et al. Esophageal atresia: prognostic classification revisited. Surgery. 2009 June;145(6):675-81.
[7] Mahoney L, Rosen R. Feeding Difficulties in Children with Esophageal Atresia. Paediatr Respir Rev. 2016 June;19:21-7.
[8] Kinoshita M, Hawkes CP, Ryan CA, Dempsey EM. Perfusion index in the very preterm infant. Acta Paediatr Oslo Nor 1992. 2013 Sept;102(9):e398-401.
[9] Oztan MO, Soyer T, Oztorun CI, Firinci B, Durakbaşa ÇU, Dokumcu Z, et al. Outcome of Very Low and Low Birth Weight Infants with Esophageal Atresia: Results of the Turkish Esophageal Atresia Registry. Eur J Pediatr Surg Off J Austrian Assoc Pediatr Surg Al Z Kinderchir. 2021 June;31(3):226-35.
[10] Hong SM, Chen Q, Cao H, Hong JJ, Huang JX. Developing a new predictive index for anastomotic leak following the anastomosis of esophageal atresia: preliminary results from a single centre. J Cardiothorac Surg. 2022 May 28;17(1):131.
[11] Stadil T, Koivusalo A, Svensson JF, Jönsson L, Lilja HE, Thorup JM, et al. Surgical treatment and major complications Within the first year of life in newborns with long-gap esophageal atresia gross type A and B - a systematic review. J Pediatr Surg. 2019 Nov;54(11):2242-9.
[12] Morini F, Conforti A, Bagolan P. Perioperative Complications of Esophageal Atresia. Eur J Pediatr Surg Off J Austrian Assoc Pediatr Surg Al Z Kinderchir. 2018 Apr;28(2):133-40.
[13] Okata Y, Maeda K, Bitoh Y, Mishima Y, Tamaki A, Morita K, et al. Evaluation of the intraoperative risk factors for esophageal anastomotic complications after primary repair of esophageal atresia with tracheoesophageal fistula. Pediatr Surg Int. 2016 Sept;32(9):869-73.
[14] Sulkowski JP, Cooper JN, Lopez JJ, Jadcherla Y, Cuenot A, Mattei P, et al. Morbidity and mortality in patients with esophageal atresia. Surgery. 2014 Aug;156(2):483-91.
[15] Shawyer AC, Pemberton J, Flageole H. Post-operative management of esophageal atresia-tracheoesophageal fistula and gastroesophageal reflux: a Canadian Association of Pediatric Surgeons annual meeting survey. J Pediatr Surg. 2014 May;49(5):716-9.
[16] Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018;9:754.
[17] Welsch T, Müller SA, Ulrich A, Kischlat A, Hinz U, Kienle P, et al. C-reactive protein as early predictor for infectious postoperative complications in rectal surgery. Int J Colorectal Dis. 2007 Dec;22(12):1499-507.
[18] Ortega-Deballon P, Radais F, Facy O, d’Athis P, Masson D, Charles PE, et al. C-reactive protein is an early predictor of septic complications after elective colorectal surgery. World J Surg. 2010 Apr;34(4):808-14.
[19] Warschkow R, Beutner U, Steffen T, Müller SA, Schmied BM, Güller U, et al. Safe and early discharge after colorectal surgery due to C-reactive protein: a diagnostic meta-analysis of 1832 patients. Ann Surg. 2012 Aug;256(2):245-50.
[20] Nurminen P, Koivusalo A, Hukkinen M, Pakarinen M. Pneumonia after Repair of Esophageal Atresia-Incidence and Main Risk Factors. Eur J Pediatr Surg Off J Austrian Assoc Pediatr Surg Al Z Kinderchir. 2019 Dec;29(6):504-9.
[21] Silvestre J, Rebanda J, Lourenço C, Póvoa P. Diagnostic accuracy of C-reactive protein and procalcitonin in the early detection of infection after elective colorectal surgery - a pilot study. BMC Infect Dis. 2014 Aug 16;14:444.
[22] Sarbinowski R, Arvidsson S, Tylman M, Oresland T, Bengtsson A. Plasma concentration of procalcitonin and systemic inflammatory response syndrome after colorectal surgery. Acta Anaesthesiol Scand. 2005 Feb;49(2):191-6.