Fixation with Purpose: A Comprehensive Review of Locking Plate Outcomes in Displaced Proximal Humerus Fractures
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
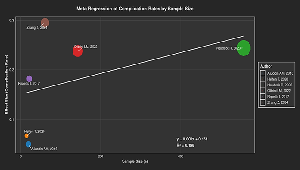
Background: Proximal humerus fracture (PHF) is common in the geriatric and young population, and locking plate fixation is a standard surgical procedure for displaced fractures. Despite technological advances, rates of complications remain unpredictable, thus its effectiveness is questioned. Aim and Objective: This study aimed to answer the significant question: “How do surgical methods, patient variables, and fracture complexity affect the complication rates of locking plate fixation, and what are the risk factors that can be modulated?” Methods: Studies published between 2014 and 2025 were searched on PubMed, Scopus and Embase. Available complication rates of locking plate fixation of adults with displaced 2-, 3-, or 4-part PHFs were considered in the studies. Thirteen studies were considered for the systematic review of which six studies were meta-analyzed for complication proportions in a random-effects model. Results: Meta-analysis of six trials (n=818) showed a mean overall complication rate of 17.9% (95% CI: 0.068–0.374). Complications were screw cut-out (4.1%), AVN (3–23%), and failure of implant (5%). The large trials showed higher rates (24-29.5%). Conclusion: Locking plate fixation has a moderate risk of complications that is dependent on fracture and patient age. Augmentation and anatomic reduction can decrease risks. Additional research is indicated for optimal protocols.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Arun Raja C J, Sajjad Ali B, Swathi N

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Burkhart KJ, Dietz SO, Bastian L, Thelen U, Hoffmann R, Müller LP. The treatment of proximal humeral fracture in adults. Deutsches Ärzteblatt International. 2013 Sep 2;110(35-36):591.
[2] Patil SN, Srinivas P, Bhadbade V. A prospective study of 30 cases of PHILOS plating for displaced proximal humeral fractures. Int J Orthop. 2017;3:86-91.
[3] Ghert M, McKee M. To operate or not to operate, that is the question: the proximal humerus fracture. Bone & Joint Research. 2016 Oct 1;5(10):490-1.
[4] Vidyadhara S, Vamsi K, Rao SK, Gnanadoss JJ, Pandian S. Use of intramedullary fibular strut graft: a novel adjunct to plating in the treatment of osteoporotic humeral shaft nonunion. International orthopaedics. 2009 Aug;33:1009-14.
[5] Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. bmj. 2021 Mar 29;372.
[6] Tan E, Lie D, Wong MK. Early outcomes of proximal humerus fracture fixation with locking plate and intramedullary fibular strut graft. Orthopedics. 2014 Sep 1;37(9):e822-7.
[7] Stone GP, Christmas KN, Mighell MA. Locking plate fixation for proximal humerus fractures-when do I use a fibular strut? Annals of Joint. 2020 Oct 15;5.
[8] Maier D, Jaeger M, Izadpanah K, Strohm PC, Suedkamp NP. Proximal humeral fracture treatment in adults. JBJS. 2014 Feb 5;96(3):251-61.
[9] Wang H, Rui B, Lu S, Luo C, Chen Y, Chai Y. Locking plate use with or without strut support for varus displaced proximal humeral fractures in elderly patients. JBJS Open Access. 2019 Jul 1;4(3):e0060.
[10] Aliuddin AM, Idrees Z, Zamir M, Najjad MK, Shah SA. Functional outcome of proximal humeral fractures treated with PHILOS plate in adults. Journal of Ayub Medical College Abbottabad. 2016 Jun 1;28(2):337-40.
[11] Dey Hazra RO, Illner J, Szewczyk K, Warnhoff M, Ellwein A, Blach RM, et al. Age-independent clinical outcome in proximal humeral fractures: 2-year results using the example of a precontoured locking plate. Journal of Clinical Medicine. 2022 Jan 14;11(2):408.
[12] Repetto I, Alessio-Mazzola M, Cerruti P, Sanguineti F, Formica M, Felli L. Surgical management of complex proximal humeral fractures: pinning, locked plate and arthroplasty: clinical results and functional outcome on retrospective series of patients. Musculoskeletal surgery. 2017 Aug;101:153-8.
[13] Jabran A, Peach C, Ren L. Biomechanical analysis of plate systems for proximal humerus fractures: a systematic literature review. Biomedical engineering online. 2018 Dec;17:1-30.
[14] Kumar R, Natarajan S, Kumar S, Kalanithi R. Outcome analysis of patients with proximal humerus fractures treated with locking plates. International Journal of Research in Orthopaedics. 2017 May;3(3):401.
[15] Launonen AP, Sumrein BO, Reito A, Lepola V, Paloneva J, Jonsson KB, et al. Operative versus non-operative treatment for 2-part proximal humerus fracture: A multicenter randomized controlled trial. PLoS medicine. 2019 Jul 18;16(7):e1002855.
[16] Helfen T, Siebenbürger G, Fleischhacker E, Gleich J, Böcker W, Ockert B. Operative treatment of 2-part surgical neck type fractures of the proximal humerus in the elderly: cement augmented locking plate PHILOS™ vs. proximal humerus nail multiloc®. Injury. 2020 Oct 1;51(10):2245-52.
[17] DeKeyser GJ, Hakim AJ, O’Neill DC, Schlickewei CW, Marchand LS, Haller JM. Biomechanical and anatomical considerations for dual plating of distal femur fractures: a systematic literature review. Archives of orthopaedic and trauma surgery. 2022 Oct;142(10):2597-609.
[18] Fleischhacker E, Siebenbürger G, Helfen T, Gleich J, Böcker W, Ockert B. Varus malposition relates to functional outcomes following open reduction and internal fixation for proximal humeral fractures: a retrospective comparative cohort study with minimum 2 years follow-up. Injury. 2021 Mar 1;52(3):506-10.
[19] Oldrini LM, Feltri P, Albanese J, Marbach F, Filardo G, Candrian C. PHILOS synthesis for proximal humerus fractures has high complications and reintervention rates: a systematic review and meta-analysis. Life. 2022 Feb 19;12(2):311.
[20] Laux CJ, Grubhofer F, Werner CM, Simmen HP, Osterhoff G. Current concepts in locking plate fixation of proximal humerus fractures. Journal of orthopaedic surgery and research. 2017 Dec;12:1-9.
[21] Banerjee M, Biswas R, Roy A. A study on the functional and radiological outcome with complications in the management of proximal humerus fractures operated with proximal humerus internal locking osteosynthesis system. Int J Res Orthop [Internet]. 2023 Apr. 28 [cited 2025 Jun. 9];9(3):553-8.
[22] Abhishek S. A prospective study of functional outcome of distal femur fractures by locking plate (Doctoral dissertation, BLDE (Deemed to be University)).2019.
[23] Neudeck R, Daferner MP, Fleischhacker E, Helfen T, Gilbert F, Böcker W, et al. Mid-term functional outcome (minimum 24 months, mean 4 years) after locking plate osteosynthesis for displaced fractures of the proximal humerus in 557 cases. Injury. 2023 Jun 1;54(6):1641-9.
[24] Dr. Vishwajeet Singh, Dr. Ronak Patel, Dr. Yogesh Pethapara, Dr. Jayant Sen, Dr. Prateek Goyal and Dr. Ankush Goyal. Investigating the functional outcomes and complications associated with open reduction and internal fixation in proximal humeral fractures locking plate: A prospective study. Int. J. Orthop. Sci. 2020;6(4):815-819.
[25] Zhang Z, Li Y, Zhao Y, Lu Y, Zhu Y, Jiang C. What are the long-term outcomes of locking plates for nonosteoporotic three-part and four-part proximal humeral fractures with a minimum 10-year follow-up period? Clinical Orthopaedics and Related Research®. 2024 May 1;482(5):831-40.
[26] Dr. Harshavardhana V, Dr. KMK Varma, Dr. Manoj Kumar AN, Dr. Samarth Arya and Dr. Pradeep D Jadhav. Study on functional outcome of proximal humerus internal locking osteosynthesis system plating for displaced proximal humerus fractures: A prospective and retrospective study. Int. J. Orthop. Sci. 2019;5(2):350-353.
[27] Bezirgan U, Kısmet M, Kıratlıoğlu Y, Yalçın M, Armangil M. Comparison of locking plate and conservative treatment in elderly patients with displaced proximal humerus fractures. International Orthopaedics. 2025 Feb 3:1-9.
[28] Aggarwal S, Bali K, Dhillon MS, Kumar V, Mootha AK. Displaced proximal humeral fractures: an Indian experience with locking plates. Journal of Orthopaedic surgery and research. 2010 Dec;5:1-8.
[29] Dr. Saranjeet Singh Jagdev, Dr. Utsav V Patel, Dr. Vinit Brahmbhatt and Dr. Dharmik Patel. Analysis and comparison of functional and radiological outcomes of distal end radius fractures managed with operative interventions. Int. J. Orthop. Sci. 2021;7(2):673-679.
[30] Hagel A, Siekmann H, Delank KS. Periprosthetic femoral fracture-an interdisciplinary challenge. Deutsches Ärzteblatt International. 2014 Sep 26;111(39):658.