Unveiling The Burden of Papilledema: A Systematic Review and Meta-Analysis of Prevalence and Risk Factors
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
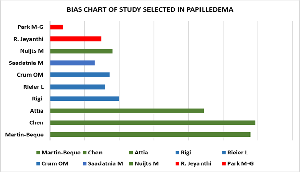
Background: Papilledema is a condition characterized by optic disc swelling due to increased intracranial pressure (ICP), pose significant risks to vision and overall neurological health. Understanding its prevalence and associated risk factors is crucial for timely diagnosis and management. Aim: To answer the question: “What is the true prevalence of papilledema across diverse populations, and what are the risk factors that most significantly contribute to its development?” This study systematically analyses the burden of papilledema by synthesizing global evidence on its prevalence and associated risk factors-such as idiopathic intracranial hypertension, obesity, age, and gender-with the ultimate goal of enabling earlier diagnosis and preventing irreversible visual loss. Methods: A comprehensive literature search was conducted across multiple databases, PubMed, Embase, and Scopus, identifying 10 relevant studies. The inclusion criteria encompassed studies that reported on the prevalence and risk factors of papilledema in diverse populations. Exclusion criteria included studies lacking clear diagnostic criteria or those not published in English. Data were extracted and analyzed using appropriate statistical methods, chi-square tests, and, p-value calculated. Results: The review revealed a wide variation in the prevalence of papilledema across studies, with significant associations with obesity, age, and gender as risk factors. Notably, idiopathic intracranial hypertension (IIH) emerged as a predominant cause of papilledema. Conclusions: The findings underscore the importance of recognizing risk factors for papilledema, particularly in high-risk populations. Enhanced awareness and early intervention strategies are essential to mitigate the potential for vision loss associated with this condition.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Anitha L, Thirumagal Vaishnavi, Abhishek Babu J, Sruthi Swaminathan, Sanjeedh Ahamed, Nabinsha J, Jamila Hameed

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Anitha L, Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Thirumagal Vaishnavi, Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Abhishek Babu J, Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Sruthi Swaminathan, Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Sanjeedh Ahamed, CRRI Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
CRRI Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Nabinsha J, CRRI Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
CRRI Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Jamila Hameed, Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
Department of Ophthalmology, Karuna Medical College, Vilayodi, Kerala, India.
[1] Karaarslan, C. Is Papilledema Really an Increasing Neuro-Ophthalmological Condition Today. Ophthalmol. Res. 2024, 7 (1), 1-7.
[2] Krispel, C. M.; Keltner, J. L.; Smith, W.; Chu, D. G.; Ali, M. R. Undiagnosed Papilledema in a Morbidly Obese Patient Population: A Prospective Study. J. Neuro-Ophthalmol. 2011, 31 (4), 310-315.
[3] Costello, F.; Hamann, S. Advantages and Pitfalls of the Use of Optical Coherence Tomography for Papilledema. Curr. Neurol. Neurosci. Rep. 2024, 24 (3), 55-64.
[4] Rigi, M.; Almarzouqi, S. J.; Morgan, M. L.; Lee, A. G. Papilledema: Epidemiology, Etiology, and Clinical Management. Eye Brain 2015, 7, 47-57.
[5] Saadatnia, M.; Pirhaji, Z. Factors Influencing the Incidence of Papilledema in Patients with Cerebral Venous Thrombosis. Adv. Biomed. Res. 2017, 6 (1), 165.
[6] Liu, K. C.; Bhatti, M. T.; Chen, J. J.; et al. Presentation and Progression of Papilledema in Cerebral Venous Sinus Thrombosis. Am. J. Ophthalmol. 2020, 213, 1-8.
[7] Crum, O. M.; Kilgore, K. P.; Sharma, R.; et al. Etiology of Papilledema in Patients in the Eye Clinic Setting. JAMA Netw. Open 2020, 3 (6), e206625.
[8] Chen, J. J.; Bhatti, M. T. Papilledema. Int. Ophthalmol. Clin. 2019, 59 (3), 3-22.
[9] Passi, N.; Degnan, A. J.; Levy, L. M. MR Imaging of Papilledema and Visual Pathways: Effects of Increased Intracranial Pressure and Pathophysiologic Mechanisms. Am. J. Neuroradiol. 2013, 34 (5), 919-924.
[10] Martín-Begué, N.; Mogas, E.; Dod, C. W.; et al. Growth Hormone Treatment and Papilledema: A Prospective Pilot Study. J. Clin. Res. Pediatr. Endocrinol. 2021, 13 (2), 146.
[11] Suh, H.; Shin, S. Y.; Park, S. H. A Case of Idiopathic Intracranial Hypertension with Papilledema Secondary to Recombinant Human Growth Hormone Treatment. J. Korean Ophthalmol. Soc. 2022, 63 (8), 735-739.
[12] Reier, L.; Fowler, J. B.; Arshad, M.; et al. Optic Disc Edema and Elevated Intracranial Pressure (ICP): A Comprehensive Review of Papilledema. Cureus 2022, 14 (5).
[13] Karanjia, R.; Sadun, A. A. Optic Atrophy and Papilledema. In Albert and Jakobiec’s Principles and Practice of Ophthalmology; Springer: Cham, 2021; pp 1-15.
[14] Nuijts, M. A.; Stegeman, I.; Porro, G. L.; et al. Ophthalmological Evaluation in Children Presenting with a Primary Brain Tumor. J. Neuro-Ophthalmol. 2022, 42 (1), e99-e108.
[15] Trobe, J. D. Papilledema: The Vexing Issues. J. Neuro-Ophthalmol. 2011, 31 (2), 175.
[16] Park, M. G.; Roh, J.; Ahn, S. H.; et al. Papilledema and Venous Stasis in Patients with Cerebral Venous and Sinus Thrombosis. BMC Neurol. 2023, 23 (1), 175.
[17] Sun, J. A.; Estrela, T.; Gise, R. Clinical Course and Visual Outcomes of Papilledema in Pediatric Cerebral Venous Sinus Thrombosis. Am. J. Ophthalmol. 2024, 263, 126-132.
[18] Jeyanthi, R.; Veeralakshmanan, S.; Gopal, B.; et al. Prevalence and Clinical Correlates of Papilledema in a Tertiary Care Hospital. Res. J. Med. Sci. 2024, 18, 307-312.
[19] Periyandavan, J.; Stephen, M.; Kasturi, N.; et al. Review on the Etiopathogenesis, Clinical Features, and Management of Pseudo-tumor Cerebri. Trop. Ophthalmol. 2024, 1 (2), 33-38.
[20] Attia, R.; Fitoussi, R.; Mairot, K.; et al. Risk Factors Associated with Progression from Papilloedema to Optic Atrophy: Results from a Cohort of 113 Patients. BMJ Open Ophthalmol. 2023, 8 (1).
[21] Athappilly, G.; García-Basterra, I.; Machado-Miller, F.; et al. Ganglion Cell Complex Analysis as a Potential Indicator of Early Neuronal Loss in Idiopathic Intracranial Hypertension. Neuro-Ophthalmol. 2019, 43 (1), 10-17.
[22] Agrawal, R.; Tidake, P. Clinical staging and visual prognosis of patients with papilloedema. Indian J. Clin. Exp. Ophthalmol. 2019, 5(1), 30-34.