Effectiveness and Safety of Co-Amoxiclav in Dental Infections: A Multicenter, Real-World Study
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
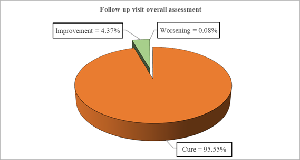
Objective: To assess the clinical effectiveness and safety of Co-Amoxiclav in the real-world treatment of dental infections. Design: Multicenter, retrospective, real world evidence study. Subjects: 4,436 adults diagnosed with dental infections Methods: This study included patients aged ≥ 18 years with a confirmed diagnosis of dental infections, who were treated with co-amoxiclav and had complete treatment documentation, including both baseline and follow-up visits. Data were extracted from medical records. The primary endpoints were the therapeutic efficacy and safety of co-amoxiclav. Statistical analysis included descriptive statistics and the paired t-test. Results: The mean age of participants was 40.23 ± 12.20 years, while the most common diagnoses was undifferentiated dental infections (52%). Co-amoxiclav 625 mg twice daily for 5–7 days was the most common regimen (40.98%), with 95.55% reporting complete symptom resolution at 7 ± 2 days. Significant reductions were observed in C-reactive protein, white blood cell count, and Visual Analog Scale pain scores (p < 0.0001), with minimal treatment-related adverse events (0.16%). Conclusion: Co-amoxiclav exhibited robust clinical effectiveness and a favourable safety profile in treating dental infections, with most patients achieving complete symptom resolution and a low incidence of adverse events.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Kumar T, Prakash J, Ahire JS, Pal A, Pawar D, Sharma A

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
Kumar T, Department of Oral Pathology, Patna Dental College and Hospital, Patna, India.
Dr. Tanoj Kumar, Department of Oral Pathology, Patna Dental College and Hospital, Patna, India.
Prakash J, The Oro Dental Clinic, SS Hospital and Research Centre, Patna, India.
Dr. Jyoti Prakash; The Oro Dental Clinic, SS Hospital and Research Centre, Patna, India.
Ahire JS, Department of Pharmacology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, India
Dr. Jayashree Ahire; Department of Pharmacology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, India.
Pal A, Medical Affairs Department, Alkem Laboratories Ltd., Mumbai, India.
Dr. Amitrajit Pal; Medical Affairs Department, Alkem Laboratories Ltd., Mumbai, India.
Pawar D, Medical Affairs Department, Alkem Laboratories Ltd., Mumbai, India.
Dr. Dattatray Pawar; Medical Affairs Department, Alkem Laboratories Ltd., Mumbai, India.
Sharma A, Medical Affairs Department, Alkem Laboratories Ltd., Mumbai, India.
Dr. Akhilesh Sharma; Medical Affairs Department, Alkem Laboratories Ltd., Mumbai, India.
[1] Słotwińska-Pawlaczyk A, Orzechowska-Wylęgała B, Latusek K, Roszkowska AM. Analysis of the clinical status and treatment of facial cellulitis of odontogenic origin in pediatric patients. International Journal of Environmental Research and Public Health [Internet]. 2023 Mar 10;20(6):4874. Available from: https://doi.org/10.3390/ijerph20064874
[2] Prakash SK. Dental abscess: A microbiological review Shweta 1. 2013; 10:585–91.
[3] Laudenbach JM, Kumar SS. Common dental and periodontal diseases. Dermatol Clin [Internet]. 2020;38(4):413–20. Available from: http://dx.doi.org/10.1016/j.det.2020.05.002
[4] Babaiwa UF, Osia EA, Ugbodaga P, Akerele JO. Epidemiology of odontogenic infections in a secondary healthcare centre in Southern Nigeria. J Pharm Biore Sources [Internet]. 2017;14(1):38. Available from: http://dx.doi.org/10.4314/jpb.v14i1.5
[5] Santacroce L, Passarelli PC, Azzolino D, Bottalico L, Charitos IA, Cazzolla AP, et al. Oral microbiota in human health and disease: A perspective. Exp Biol Med (Maywood) [Internet]. 2023;248(15):1288–301. Available from: http://dx.doi.org/10.1177/15353702231187645
[6] Meinen A, Reuss A, Willrich N, Feig M, Noll I, Eckmanns T, et al. Antimicrobial resistance and the spectrum of pathogens in dental and oral-maxillofacial infections in hospitals and dental practices in Germany. Front Microbiol [Internet]. 2021; 12:676108. Available from: http://dx.doi.org/10.3389/fmicb.2021.676108
[7] Osuh ME, Oke GA, Lilford RJ, Osuh JI, Harris B, Owoaje E, et al. Systematic review of oral health in slums and non-slum urban settings of Low and Middle-Income Countries (LMICs): Disease prevalence, determinants, perception, and practices. PLoS One [Internet]. 2024;19(11):e0309319. Available from: http://dx.doi.org/10.1371/journal.pone.0309319
[8] Pandey P, Nandkeoliar T, Tikku AP, Singh D, Singh MK. Prevalence of dental caries in the Indian population: A systematic review and meta-analysis: A systematic review and meta-analysis. J Int Soc Prev Community Dent [Internet]. 2021;11(3):256–65. Available from: http://dx.doi.org/10.4103/jispcd.JISPCD_42_21
[9] Osuh ME, Oke GA, Lilford RJ, Owoaje E, Harris B, Taiwo OJ, et al. Prevalence and determinants of oral health conditions and treatment needs among slum and non-slum urban residents: Evidence from Nigeria. PLOS Glob Public Health [Internet]. 2022;2(4):e0000297. Available from: http://dx.doi.org/10.1371/journal.pgph.0000297
[10] Jain N, Dutt U, Radenkov I, Jain S. WHO’s global oral health status report 2022: Actions, discussion and implementation. Oral Dis [Internet]. 2024;30(2):73–9. Available from: http://dx.doi.org/10.1111/odi.14516
[11] Li X, Kolltveit KM, Tronstad L, Olsen I. Systemic diseases caused by oral infection. Clin Microbiol Rev [Internet]. 2000;13(4):547–58. Available from: http://dx.doi.org/10.1128/cmr.13.4.547
[12] Thompson W, Teoh L, Hubbard CC, Marra F, Patrick DM, Mamun A, et al. Patterns of dental antibiotic prescribing in 2017: Australia, England, United States, and British Columbia (Canada). Infect Control Hosp Epidemiol [Internet]. 2022;43(2):191–8. Available from: http://dx.doi.org/10.1017/ice.2021.87
[13] Contaldo M, Ambrosio F, Ferraro GA, Stasio D, Palo D, Serpico MP, et al. Antibiotics in Dentistry: A Narrative Review of the Evidence beyond the Myth.20(11):6025. 2023;20.
[14] Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. P T. 2015;40(4):277–83.
[15] Ahmadi H, Ebrahimi A, Ahmadi F. Antibiotic therapy in dentistry. Int J Dent [Internet]. 2021; 2021:6667624. Available from: http://dx.doi.org/10.1155/2021/6667624
[16] Bush K, Bradford PA. Β-lactams and β-lactamase inhibitors: An overview. Cold Spring Harb Perspect Med [Internet]. 2016;6(8). Available from: http://dx.doi.org/10.1101/cshperspect.a025247
[17] Tancawan AL, Pato MN, Abidin KZ, Asari ASM, Thong TX, Kochhar P, et al. Amoxicillin/clavulanic acid for the treatment of odontogenic infections: A randomised study comparing efficacy and tolerability versus clindamycin. Int J Dent [Internet]. 2015;2015:472470. Available from: http://dx.doi.org/10.1155/2015/472470
[18] Adriaenssen CF. Comparison of the efficacy, safety and tolerability of azithromycin and co-amoxiclav in the treatment of acute periapical abscesses. J Int Med Res [Internet]. 1998;26(5):257–65. Available from: http://dx.doi.org/10.1177/030006059802600506
[19] Sulejmanagić N, Sulejmanagić H, Ljutović Z, Salihagić D, Sijercić M. Combined application of amoxicillin and clavulanic acid after oral surgical interventions. Bosn J Basic Med Sci [Internet]. 2005;5(1):61–8. Available from: http://dx.doi.org/10.17305/bjbms.2005.3337
[20] Halling F, Neff A, Heymann P, Ziebart T. Trends in antibiotic prescribing by dental practitioners in Germany. J Craniomaxillofac Surg [Internet]. 2017;45(11):1854–9. Available from: http://dx.doi.org/10.1016/j.jcms.2017.08.010
[21] Choudhury J, Makkar A, Sharma V, Karamath SP, Parmar V, Kumar J P, et al. A real-world perspective of co-amoxiclav prescription pattern with probiotics for pediatric patients with respiratory tract infections: Results of quantitative and qualitative approach in Indian outpatient settings. Cureus [Internet]. 2023;15(3): e36269. Available from: http://dx.doi.org/10.7759/cureus.36269
[22] Sobottka I, Cachovan G, Stürenburg E, Ahlers MO, Laufs R, Platzer U, et al. In vitro activity of moxifloxacin against bacteria isolated from odontogenic abscesses. Antimicrob Agents Chemother [Internet]. 2002;46(12):4019–21. Available from: http://dx.doi.org/10.1128/AAC.46.12.4019-4021.2002
[23] Robertson D, Smith AJ. The microbiology of the acute dental abscess. J Med Microbiol [Internet]. 2009;58(Pt 2):155–62. Available from: http://dx.doi.org/10.1099/jmm.0.003517-0
[24] AlShammari A, AlSaleh S, AlKandari A, AlSaqabi S, AlJalahmah D, AlSulimmani W, et al. The association between dental caries and serum crp in the us adult population: evidence from NHANES 2015-2018. BMC Public Health [Internet]. 2024;24(1):2210. Available from: http://dx.doi.org/10.1186/s12889-024-19681-6
[25] Lim MY, Kim J-H, Nam Y-D. Oral microbiome correlates with selected clinical biomarkers in individuals with no significant systemic disease. Front Cell Infect Microbiol [Internet]. 2023; 13:1114014. Available from: http://dx.doi.org/10.3389/fcimb.2023.1114014
[26] Huang H, Li L, Wu M, Liu Z, Zhao Y, Peng J, et al. Antibiotics and antibiotic-associated diarrhea: a real-world disproportionality study of the FDA adverse event reporting system from 2004 to 2022. BMC Pharmacol Toxicol [Internet]. 2023;24(1):73. Available from: http://dx.doi.org/10.1186/s40360-023-00710