Assessment of Sleep Quality and Mental Health Status Among 1st Year MBBS Students of a Tertiary Care Hospital in West Bengal: A Cross-sectional Observational Study
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
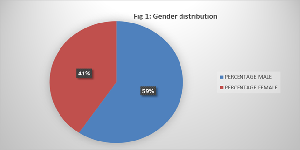
Objectives: To assess the sleep pattern and mental health status among 1st year medical students. - To find out any relationship between them. Design: Cross-sectional observational study. Subjects: Apparently healthy newly admitted 1st year MBBS student of Bankura Sammilani Medical College aged between 18-25 years of age. Methodology: After obtaining institutional ethical clearance and written informed consent from study participants, this study was conducted over a period of 3 months. The students with pre-existing mental health disorders, sleep apnoea and not willing to give consent were excluded from the study. Sleep quality and mental health status were measured by administering Pittsberg Sleep Quality Index and DASS-21 scale respectively. Results: A total of 133 students responded to the questionnaires with mean age of 20.09 ± 1.33 years and 60-40% male-female distribution. The mean PSQI score was found to be 5.09±2.76 (Score ≥ 5 indicates poor quality sleep pattern). The mean score for depression, anxiety and stress from Dass 21 score indicate mild anxiety, moderate depression and mild stress among them. Furthermore, Spearman rank correlation showed a moderate correlation between sleep quality and mental health among the students. Conclusion: Our study may be helpful to assess and screen the medical students having altered sleep pattern and mental health issues at the earliest.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dr Binita Mondal, Dr Maumita Das, Dr Debdeep Dasgupta, Dr Arindam Ghosh

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Van Dongen HPA, Maislin G, Mullington JM, Dinges DF. The Cumulative Cost of Additional Wakefulness: Dose-Response Effects on Neurobehavioral Functions and Sleep Physiology From Chronic Sleep Restriction and Total Sleep Deprivation. Sleep. 2003 Mar;26(2):117-26.
[2] Kushida CA, Nichols DA, Simon RD, Young T, Grauke JH, Britzmann JB, et al. Symptom-Based Prevalence of Sleep Disorders in an Adult Primary Care Population. Sleep and Breathing. 2000 Jan;4(1):11-5.
[3] Jewett ME, Dijk DJ, Kronauer RE, Dinges DF. Dose-response Relationship Between Sleep Duration and Human Psycho-motor Vigilance and Subjective Alertness. Sleep. 1999 Mar;22(2):171-9.
[4] Veldi M, Aluoja A, Vasar V. Sleep quality and more common sleep-related problems in medical students. Sleep Medicine. 2005 May 1;6(3):269-75.
[5] Loayza H MP, Ponte TS, Carvalho CG, Pedrotti MR, Nunes PV, Souza CM, et al. Association between mental health screening by self-report questionnaire and insomnia in medical students. Arquivos De Neuro-Psiquiatria. 2001 Jun 1;59(2-A):180-5.
[6] Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, et al. Sleep Disturbances among Medical Students: A Global Perspective. Journal of Clinical Sleep Medicine. 2015 Jan 15;11(1).
[7] Hershner S, Chervin R. Causes and Consequences of Sleepiness among College Students. Nature and Science of Sleep. 2014 Jun 23;6(6):73-84.
[8] Oginska H, Pokorski J. Fatigue and mood correlates of sleep length in three age-social groups: School children, students, and employees. Chronobiology International. 2006;23(6):1317-28.
[9] Lund HG, Reider BD, Whiting AB, Prichard JR. Sleep Patterns and Predictors of Disturbed Sleep in a Large Population of College Students. Journal of Adolescent Health. 2010;46(2):124-32.
[10] Núñez-Regueiro M. Yaşlı Kadınlarda Üreme Sağlığı. DergiPark (Istanbul University). 2020 Feb 1;1(1).
[11] Buboltz WC, Brown FC. Sleep Habits and Patterns of College Students: A Preliminary Study. Journal of American College Health. 2016;50(3):131-5.
[12] Strine TW, Chapman DP. Associations of frequent sleep insufficiency with health-related quality of life and health behaviors. Sleep Medicine. 2005 Jan;6(1):23-7.
[13] Gupta N, Garg S, Arora K. Pattern of mobile phone usage and its effects on psychological health, sleep, and academic performance in students of a medical university. National Journal of Physiology, Pharmacy and Pharmacology. 2016;6(2):132.
[14] Telzer EH, Fuligni AJ, Lieberman MD, Galván A. The effects of poor quality sleep on brain function and risk taking in adolescence. NeuroImage. 2013 May; 71:275-83.
[15] Turk J. Sleep disorders in children and adolescents with learning disabilities and their management. Advances in Mental Health and Learning Disabilities. 2010 Mar 15;4(1):50-9.
[16] Rezaei O, Mokhayeri Y, Haroni J, Rastani MJ, Sayadnasiri M, Ghisvand H, et al. Association between sleep quality and quality of life among students: a cross sectional study. International Journal of Adolescent Medicine and Health. 2017 Sep 15;0(0).
[17] Waqas A, Khan S, Sharif W, Khalid U, Ali A. Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. PeerJ. 2015 Mar 12;3:e840.
[18] Sethia R, Sharma G, Shekhawat K, Aacharya A, Acharya R, Meena RR. Study of perceived stress and stressors among undergraduate medical students. International Journal Of Community Medicine And Public Health. 2019 Mar 27;6(4):1690.
[19] Wong JGWS, Patil NG, Beh SL, Cheung EPT, Wong V, Chan LC, et al. Cultivating psychological well-being in Hong Kong’s future doctors. Medical Teacher. 2005 Dec;27(8):715-9.
[20] Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders. 2009 Apr;114(1-3):163-73.
[21] Tafoya SA, Aldrete-Cortez V, Ortiz S, Fouilloux C, Flores F, Monterrosas AM. Resilience, sleep quality and morningness as mediators of vulnerability to depression in medical students with sleep pattern alterations. Chronobiology International. 2018 Dec 4;36(3):381-91.
[22] Paunio T, Korhonen T, Hublin C, Partinen M, Koskenvuo K, Koskenvuo M, et al. Poor sleep predicts symptoms of depression and disability retirement due to depression. Journal of Affective Disorders. 2015 Feb; 172:381-9.
[23] Brougham RR, Zail CM, Mendoza CM, Miller JR. Stress, Sex Differences, and Coping Strategies Among College Students. Current Psychology. 2009 Feb 11;28(2):85-97.
[24] Shah M, Hasan S, Malik S, Sreeramareddy CT. Perceived Stress, Sources and Severity of Stress among medical undergraduates in a Pakistani Medical School. BMC Medical Education. 2010 Jan 15;10(1).
[25] Sahoo S, Khess CRJ. Prevalence of Depression, Anxiety, and Stress Among Young Male Adults in India. The Journal of Nervous and Mental Disease. 2010 Dec;198(12):901-4.
[26] Paula W de, Breguez GS, Machado EL, Meireles AL. Prevalence of anxiety, depression, and suicidal ideation symptoms among university students: a systematic review. Brazilian Journal of Health Review. 2020;3(4):8739-56.
[27] Abdulrahman Almalki, Shehata M, Siddiqui K, Hamzah Albulushi, Nawaf Alshehri, Aldumri A, et al. Sleep Quality Among a Sample of Medical Students and the Association with Academic Performance: An Updated Data. Journal of Epidemiology and Global Health. 2025 Jan 27;15(1).
[28] Binjabr MA, Alalawi IS, Alzahrani RA, Albalawi OS, Hamzah RH, Ibrahim YS, et al. The Worldwide Prevalence of Sleep Problems Among Medical Students by Problem, Country, and COVID-19 Status: a Systematic Review, Meta-analysis, and Meta-regression of 109 Studies Involving 59427 Participants. Current Sleep Medicine Reports. 2023 Jun 3;9.
[29] Mishra J, Panigrahi A, Samanta P, Dash K, Mahapatra P, Behera MR. Sleep quality and associated factors among undergraduate medical students during Covid-19 confinement. Clinical Epidemiology and Global Health. 2022 May; 15:101004.
[30] Massarat Begum, Dimple Siri Chandana Puchakayala. Study to determine prevalence of poor sleep quality and its correlation with sleep hygiene practices among medical students. Asian Journal of Medical Sciences. 2022 Sep 1;13(9):151-5.
[31] Quek TTC, Tam WWS, Tran BX, Zhang M, Zhang Z, Ho CSH, et al. The Global Prevalence of Anxiety Among Medical Students: A Meta-Analysis. International Journal of Environmental Research and Public Health. 2019 Jul 31;16(15):2735.
[32] Almutairi AG, Nuran Mazen Baabbad, Almaha Abdullah Alhumaidan, Aljawharah Mohammed Alshahrani, Alanoud Ibrahim Alabdulkarim, Naif Alsughier. Prevalence and factors causing test anxiety among medical students. Middle East Current Psychiatry. 2024 Jun 28;31(1).
[33] Gupta P, Nitin Panwar, Verma A, Debnath A. Prevalence of anxiety among medical students in a northern state of India and gaps in mental health service utilization: a cross-sectional study. The Evidence. 2024 May 29;3(1).
[34] Ebrahim OS, Hanan Ali Sayed, Samah Rabei, Hegazy N. Perceived stress and anxiety among medical students at Helwan University: A cross-sectional study. Journal of Public Health Research. 2024 Jan 1;13(1).
[35] Feng P, Becker B, Zheng Y, Feng T. Sleep deprivation affects fear memory consolidation: bi-stable amygdala connectivity with insula and ventromedial prefrontal cortex. Social Cognitive and Affective Neuroscience. 2017 Dec 20;13(2):145-55.
[36] Li Y, Gu S, Wang Z, Li H, Xu X, Zhu H, et al. Relationship Between Stressful Life Events and Sleep Quality: Rumination as a Mediator and Resilience as a Moderator. Frontiers in Psychiatry. 2019 May 27;10.
[37] Hall. Pocket Companion to Guyton and Hall Textbook Of Medical Physiology. S.L.: Elsevier; 2020.
[38] Leproult R, Copinschi G, Buxton O, Van Cauter E. Sleep loss results in an elevation of cortisol levels the next evening. Sleep. 1997 Oct 1;20(10):865-70.