Epiploic Appendagitis Causing Small Bowel Obstruction - A Rare Case Report
Authors
##plugins.themes.bootstrap3.article.main##
Abstract
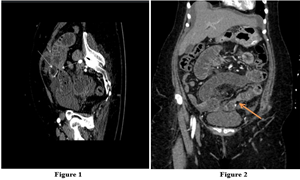
Background: Small bowel obstruction (SBO) remains a frequently encountered cause of hospital admission and surgical intervention. While postoperative adhesions are the predominant aetiology, other causes including hernias, neoplasms, and inflammatory conditions must be considered. Epiploic appendagitis (EA), though rare, can lead to SBO by causing localised inflammation, torsion, or adhesion formation. Prompt diagnosis is essential to avoid unnecessary surgery and to enable appropriate management. Case Report: A 62-year-old woman presented with symptoms of diffuse abdominal pain, vomiting, and obstipation. With no previous history of abdominal surgery, imaging studies revealed a subacute small bowel obstruction. A diagnostic laparoscopy identified a calcified epiploic appendage from the sigmoid colon mesentery, which was compressing the distal jejunum. The appendage was resected. Histopathology confirmed fat necrosis and calcification, consistent with epiploic appendagitis. The patient made a full recovery and was discharged by postoperative day three. Conclusion: This case highlights the importance of considering epiploic appendagitis as a rare but significant differential in causes of SBO, especially in patients with virgin abdomen. Early recognition and laparoscopic management can lead to excellent outcomes.
##plugins.themes.bootstrap3.article.details##
Copyright (c) 2025 Dhiliphan A M, Naveen Alexander, Koralla Sai Prathyusha

This work is licensed under a Creative Commons Attribution 4.0 International License.
Creative Commons License All articles published in Annals of Medicine and Medical Sciences are licensed under a Creative Commons Attribution 4.0 International License.
[1] Miller G., Boman J., Shrier I., Gordon P. H. Etiology of small bowel obstruction. American Journal of Surgery. 2000;180(1):33-36. doi: 10.1016/S0002-9610(00)00407-4. [DOI] [PubMed] [Google Scholar]
[2] Singh A. K., Gervais D. A., Hahn P. F., Sagar P., Mueller P. R., Novelline R. A. Acute epiploic appendagitis and its mimics. Radiographics. 2005;25(6):1521-1534. doi: 10.1148/rg.256055030. [DOI] [PubMed] [Google Scholar]
[3] Huang K., Waheed A., Juan W., Misra S., Alpendre C., Jones S. Acute epiploic appendagitis at the tip of the appendix mimicking acute appendicitis: a rare case report with literature review. World Journal of Gastrointestinal Surgery. 2019;11(8):342-347. doi: 10.4240/wjgs.v11.i8.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
[4] Lee M. P. Small bowel obstruction due to epiploic appendagitis. The American Journal of Gastroenterology. 1990;85(6):771-772. [PubMed] [Google Scholar]
[5] Nemoto H., Yoshizawa Y., Hibi K., et al. Strangulation caused by a small bowel epiploic appendage: report of a case. Case Reports in Gastroenterology. 2008;2(2):214-218. doi: 10.1159/000135609. [DOI] [PMC free article] [PubMed] [Google Scholar]
[6] Carmichael D. H., Organ C. H., Jr. Epiploic Disorders. Archives of Surgery. 1985;120(10):1167-1172. doi: 10.1001/archsurg.1985.01390340063012. [DOI] [PubMed] [Google Scholar]
[7] Nugent J. P., Ouellette H. A., O’Leary D. P., Khosa F., Nicolaou S., McLaughlin P. D. Epiploic appendagitis: 7-year experience and relationship with visceral obesity. Abdominal Radiology. 2018;43(7):1552-1557. doi: 10.1007/s00261-017-1355-5. [DOI] [PubMed] [Google Scholar]
[8] Dockerty M. B., Lynn T. E., Waugh J. M. A clinicopathologic study of the epiploic appendages. Surgery, Gynecology & Obstetrics. 1956; 103:423-433. [PubMed] [Google Scholar]
[9] de Brito P., Gomez M. A., Besson M., Scotto B., Huten N., Alison D. Frequency and epidemiology of primary epiploic appendagitis on CT in adults with abdominal pain. Journal de Radiologie. 2008;89(2):235-243. doi: 10.1016/s0221-0363(08)70399-8. [DOI] [PubMed] [Google Scholar]
[10] Vázquez G. M., Manzotti M. E., Alessandrini G., Lemos S., Perret M. C., Catalano H. N. Primary epiploic appendagitis: clinical features in 73 cases. Medicina (B Aires) 2014;74(6):448-450. [PubMed] [Google Scholar]
[11] Almeida A. T., Melão L., Viamonte B., Cunha R., Pereira J. M. Epiploic appendagitis: an entity frequently unknown to clinicians-diagnostic imaging, pitfalls, and look-alikes. American Journal of Roentgenology. 2009;193(5):1243-1251. doi: 10.2214/AJR.08.2071. [DOI] [PubMed] [Google Scholar]
[12] Nejadhamzeeigilani H. The central dot sign of epiploic appendagitis. Abdominal Radiology. 2019;44(2):802-803. doi: 10.1007/s00261-018-1769-8. [DOI] [PubMed] [Google Scholar]
[13] Suresh Kumar V. C., Mani K. K., Alwakkaa H., Shina J. Epiploic appendagitis: an often-misdiagnosed cause of acute abdomen. Case Reports in Gastroenterology. 2019;13(3):364-368. doi: 10.1159/000502683. [DOI] [PMC free article] [PubMed] [Google Scholar]
[14] Catena F., Simone B., Coccolini F., Di Saverio S., Sartelli M., Ansaloni L. Bowel obstruction: a narrative review for all physicians. World Journal of Emergency Surgery. 2019;14(1): p. 20. doi: 10.1186/s13017-019-0240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]